Jeudi, 25 novembre 2021
-
08:00 – 08:45
Enregistrement
-
08:45 – 09:15
Gartensaal 1 A-C
Ouverture conjointe
U. Hug, Luzern (CH) / P. Kammermann, Bern (CH) / S. Rosca-Furrer, La-Chaux-de-Fonds (CH)Lassen Sie sich überraschen!
-
09:30 – 10:30
Gartensaal 1 A-C
Communications libres I A
J. Beaulieu, Genève (CH) / T. Franz, Uster (CH)To operate or not to operate: When is it best to perform a PIP arthroplasty?
M. Marks1, M. Oyewale1, B. Steiger1, S. Neumeister1, S. Schindele1, D. B. Herren1 (1Zürich)
Show text
Background: There is an ongoing discussion about the optimal timing of surgery for patients with proximal interphalangeal (PIP) joint osteoarthritis (OA). It would be useful to know at which level of preoperative symptoms patients should be operated on to achieve the potentially best postoperative result.
Objective: The objective of this study was to define clinically relevant preoperative thresholds at which patients with PIP joint OA have the greatest chance to achieve a minimal important change (MIC) and a patient acceptable symptom state (PASS) one year after surgery.
Methods: Data from our prospective registry including patients with PIP joint OA who underwent arthroplasty for this condition and who had a 1-year follow-up were analysed. Patients were examined before and 1.5, 3, and 12 months after surgery. They indicated pain on a numeric rating scale (0-10) and completed the brief Michigan Hand Questionnaire (MHQ, 0-100). Active range of motion (ROM) of the affected PIP joint was measured. Radial rays (index and middle finger) and ulnar rays (ring and little finger) were analysed separately. The preoperative thresholds, which are predictive to achieve the MIC and PASS, were determined using receiver operating characteristics (ROC) curves.
Results: We included 214 patients with 263 fingers and a mean age of 68 (±10) years. Patients have the highest chance to achieve a MIC and PASS, if they are operated with preoperative pain at rest between 2.5 and 6.5, pain during activities of about 6.5, a brief MHQ score of about 42, ROM between 46° and 49° (radial rays), and ROM of 46° to 63° (ulnar rays). Within these reference values, patients have the greatest chance of achieving a subjectively relevant change and an acceptable symptom state.
Conclusion: The determined thresholds may help the surgeon in the preoperative decision-making process to decide for or against a surgical intervention and to explain the probability of achieving sufficient postoperative symptom relief to the patient. The findings substantiate our experience of patients being operated on too early or too late in the course of the disease.
Thumb interphalangeal joint replacement with a surface replacing implant: a prospective study
S. Schindele1, M. Marks1, D. B. Herren1 (1Zürich)
Show text
Objective: The objective of this study was to evaluate the 1-year patient-reported and clinical outcomes of thumb interphalangeal (IP) joint arthroplasty using a surface replacing implant (CapFlex-PIP, KLS Martin, Germany).
Methods: In this prospective pilot study, we included patients who received a CapFlex-PIP implant at the thumb IP joint. Patients rated their satisfaction with the treatment outcome on a 5-point Likert scale. They completed the brief Michigan Hand Outcomes Questionnaire (MHQ) and rated their pain on a numeric rating scale (0-10). Range of motion (ROM) of the thumb IP joint and key pinch were measured.
Results: Twelve patients with a median age of 67 years (range 53-80 years) were included. The brief MHQ increased from median 41 points before surgery to 50 at 1 year. Pain decreased from median 5.5 before surgery to 1.0 at 1 year. Total range of IP joint motion was 40° at 1 year. Key pinch increased form median 4kg before surgery to 5gk one year later. Seven patients were satisfied and five were unsatisfied with the treatment outcome at 1 year. Among the unsatisfied patients were heavy manual workers and one patient with severe systemic lupus erythematosus. One dislocated implant was revised to an arthrodesis.
Conclusion: Based on the inconsistent results, we conclude that thumb IP arthroplasty with a surface gliding implant is rarely indicated, but could be an alternative for patients attaching great importance on mobility and precision tasks. For patients who either have high demands for a powerful pinch grip, the high physical demands of a manual job or a rheumatoid disease, thumb IP joint arthrodesis should be preferred.
Outcomes and recommendations for revision of thumb carpometacarpal resection arthroplasty
D. B. Herren1, N. Fuchs1, S. Schindele1, M. Marks1 (1Zürich)
Show text
Objective: There a no clear guidelines advocating how patients with residual symptoms after thumb carpometacarpal (CMC I) resection arthroplasty should be treated further. The aims of our study were to (1) investigate the medium-term results of CMC I revision interventions, and (2) define a revision concept including diagnostic recommendations for different residual symptoms after resection arthroplasty.
Methods: Patients who had undergone primary trapeziectomy with or without tendon suspension and interposition followed by at least one revision surgery more than 12 months before were invited for a clinical follow-up examination. Patients completed the brief Michigan Hand Outcomes Questionnaire (MHQ) and rated pain on a numeric rating scale (0-10).
Results: Twenty-four patients with 25 affected thumbs were examined on average 5.5 years after their last revision surgery. Mean pain at rest was 1.6 (SD 2.0), pain during daily activities was 2.7 (SD 2.7) and the brief MHQ score was 63 (SD 19). Seventeen patients (68%) indicated that their thumb was better than before primary surgery. The four relevant subgroups encompassing the reasons for revision were (Figure 1): Impingement of the MC I (main reason), scaphotrapezoidal (ST) arthritis, flexor carpi radialis tendinitis and problems caused by other joints.
Conclusion: Although 68% of patients indicated that their thumb was better than before primary surgery, the outcome after revision surgery was less favourable than that reported for primary resection arthroplasty. Our revision algorithm suggests that the main reason for revision — symptomatic impingement of the MC I — should be first treated with a steroid infiltration. If symptoms persist, a computer tomography examination is recommended to confirm and localise these problems. In most cases, the two corresponding bones causing the impingement give rise to marks in the form of either sclerosis, abrasion, or cystic bone changes. Upon confirmation, a resection of the MC I base and ST joint is recommended. An existing interposition should be revised, or a new interposition should be used preferably with an autologous tendon or alternately with an allograft.
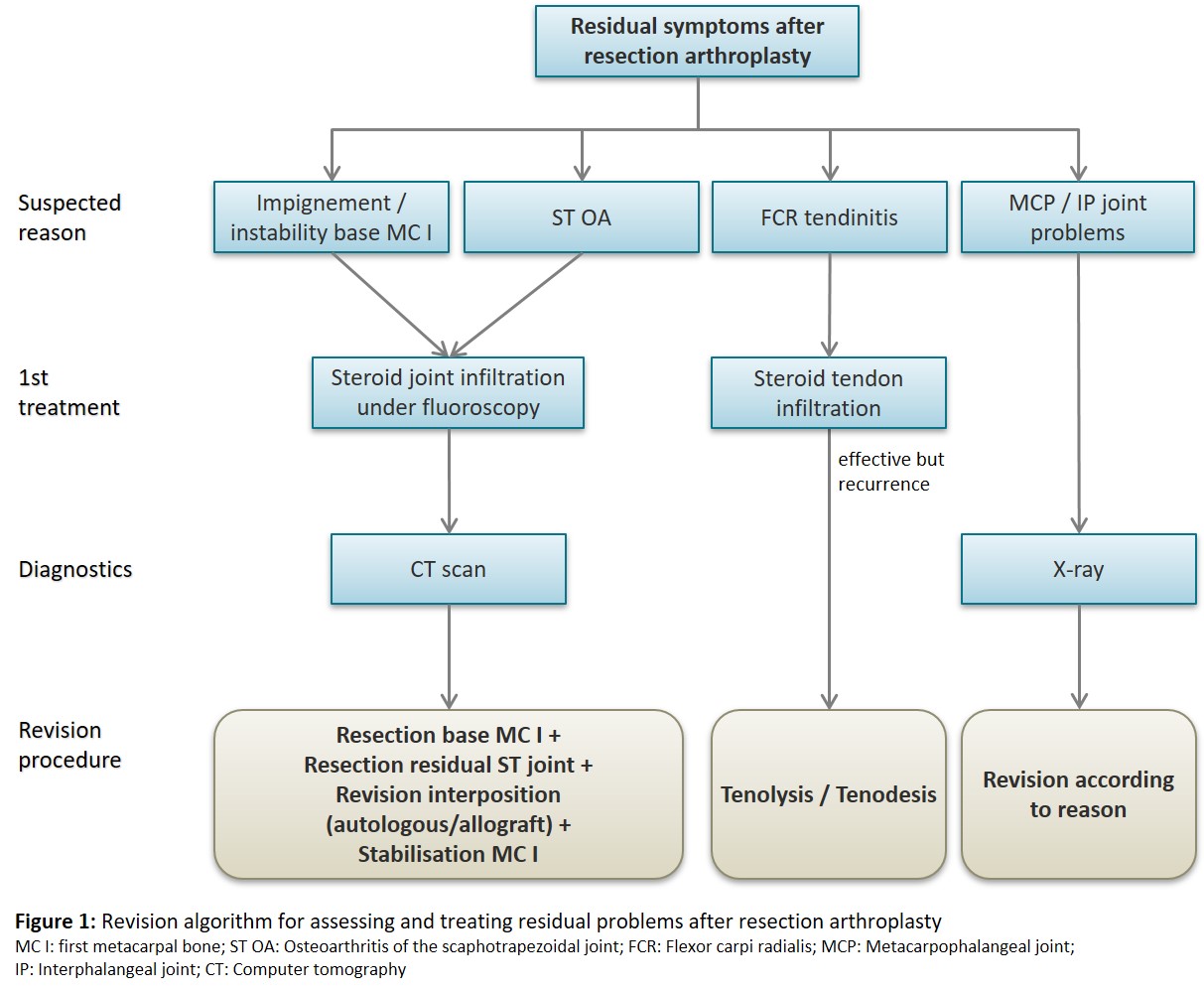
Figure 1: Revision algorithm for assessing and treating residual problems after resection arthroplasty To resect or suture the capsule in thumb carpometacarpal joint implant arthroplasty?
V. Reischenböck1, M. Oyewale1, M. Marks1, S. Schindele1, D. B. Herren1 (1Zürich)
Show text
Background: To further facilitate the rehabilitation and enhance range of motion (ROM) of the thumb carpometacarpal (CMC) joint, it has been suggested to perform capsular resection in total joint arthroplasties instead of traditional capsular repair.
Objective: We aimed to compare the effects of CMC I arthroplasty with capsular resection (CR) versus capsular suture (CS) on patients operated with the Touch® (KeriMedical) CMC I total arthroplasty.
Methods: Patients with a Touch® CMC implant that are prospectively recorded in our registry complete the brief Michigan Hand Outcomes Questionnaire (brief MHQ; score 0-100), report their pain levels at rest (Numeric Rating Scale; 0-10), and have their thumb opposition (Kapandji score) and key pinch strength assessed. Statistical analyses include t-tests to compare within- and between group differences and a linear regression model to adjust for baseline status if baseline data differed between the groups (e.g. key pinch and pain).
Results: 66 patients with a follow-up of at least one year underwent an implant arthroplasty for CMC I osteoarthritis. In 39 patients the capsule was resected and in 27 patients it was sutured. The brief MHQ scores increased from 45 (±14) at baseline to 85 (±18; p≤0.05) after one year in the CR group and from 47 (±14) to 76 (±21; p≤0.05) in the CS group. The Kapandji scores increased from 8.6 (±1.9) to 9.9 (±0.3, p<0.05) in the CR group and from 8.5 (±2.6) to 9.4 (±1.4) in the CS group. These results were significantly better in the CR group. The linear regression model analysis, on the other hand, showed no significant influence of the group allocation on the increase in pinch strength from 5kg (±3) before surgery to 7kg (±4; p≤0.05) in the CR group and from 4kg (±2.5) to 6kg (±2; p≤0.05) in the CS group. Similar findings were observed for pain levels.
In each group, one implant had to be revised and converted to a resection-suspension-interposition arthroplasty. A causal relationship between the handling of the capsule and these complications is unlikely.
Conclusion: These findings confirm that patients recover well after the implantation of the Touch® CMC I total arthroplasty for CMC I osteoarthritis. Capsular resection shows promising results by indicating better overall hand function, although improvement of pain and pinch strength after one year shows no significant between group differences.Analysis of CMC I joint kinematics using 4D-CT imaging in vivo - an observational study
A. Gübeli1, M. Keller1, I. Dobbe2, P. Honigmann1 (1Liestal; 2Amsterdam NL)
Show text
Background: Four-dimensional computer tomography (4D-CT) imaging is spreading in the medical field and has recently reached the field of hand surgery. Analysis of the thumb carpometacarpal (CMC I) joint using this technique however is limited to a few feasability studies or studies with a very small amount of volunteers.1-2 Our aim is to visualize the CMC I joint kinematics and change of articular surface contact area during motion using dynamic distance mapping.
Method: We conducted a 4D-CT scan of a cadaver CMC I joint to test the imaging protocol and estimate the radiation dose.
20 volunteers without symptoms at the thumb CMC joint were recruited for this study. They were trained to perform a thumb opposition and retropulsion movement by a hand surgeon smoothly over a period of 10 seconds.
4D-CT scans were performed at a temporal resolution of 5 frames per second, resulting in 50 frames for each movement (10 seconds of movement duration). The effective radiation dose of one 4D-CT scan with the duration of 10 seconds was approximately 0.176 mSv.
The trapeziometacarpal joint surface was divided into a grid and the distance between the articular surfaces of the metacarpal bone and the trapezium during motion was calculated for each square of the grid, resulting in a coloured pattern visualizing the contact area of the joint (Fig. 1).
Results and conclusion: We were able to optimize the visualization and understanding of CMC I joint kinematics, discovering CMC I joint phenotypes and possible causes for the development of CMC I joint osteoarthritis. Compared to earlier studies on this topic, we analysed thumb opposition motion in vivo with real 4D-CT imaging compared to 3D-CT scans at static endpoints and the analysis was conducted in higher resolution using absolute distance for the proximity calculation.
References:
1. Goto et al. In vivo pilot study evaluating the thumb carpometacarpal joint during circumduction. Clin Orthop Relat Res. 2014;472(4):1106–13.
2. Wang et al. Quantitative analysis of in-vivo thumb carpometacarpal joint kinematics using four-dimensional computed tomography. J Hand Surg Eur Vol. 2018;43(10):1088–97.
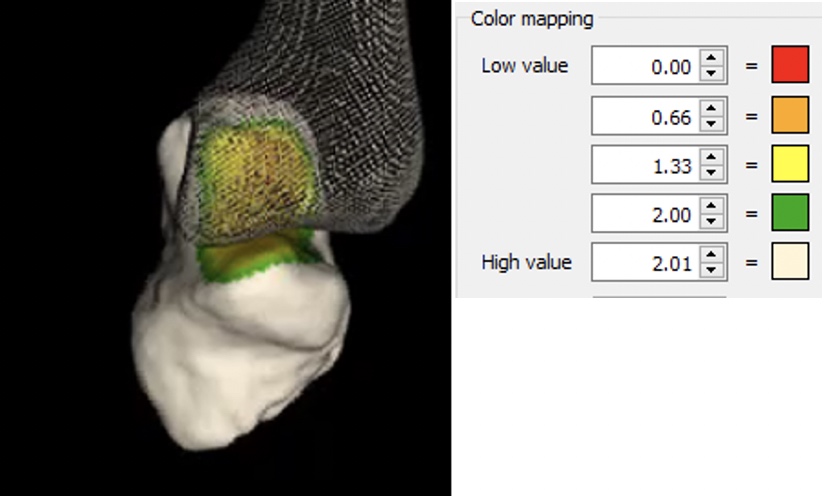
Fig. 1 Color mapping of the articular surface distance (in millimeters) in the CMC I joint during thumb opposition Radiographic landmarks for centering the trapezial cup in trapeziometacarpal joint arthroplasty
L. Auberson1, L. Athlani2, J. Y. Beaulieu1 (1Genève; 2Nancy FR)
Show text
Introduction : Trapeziometacarpal (TMC) total joint arthroplasty is a surgical option to treat TMC osteoarthritis that have not responded to conservative treatment. Generally, clinical results are good with significant pain reduction and functional thumb range of motion. However, one of the main complications is cup loosening. Various authors highlighted the importance of correct cup positioning to minimize the risk of loosening. They suggest the importance of having a satisfactory bone support on each side of the cup allowing a high osteointegration. Thereby, some of them propose that the prosthetic cup in the trapezium should be placed in the center of the distal articular surface of the trapezium. We hypothesize that the center of the distal articular surface of the trapezium does not match with the middle of the trapezium width. Based on radiographs, we sought to evaluate those two radiographic landmarks with an aim to identify the most reliable solution for centering the trapezial component.
Material and method : We performed a retrospective review of standard anteroposterior and lateral x-rays of the thumb from 80 patients. On the frontal x-rays, we measured the distal articular surface of the trapezius and the width of the trapezius. We compared the respective midpoints of these two distances, as radiographic centering marks for the positioning of a 9 mm cup (corresponding to the diameter of the trapezial cup of the Touch® implant (KeriMedical)). We measured the distance between the radial end of each segment and the radial edge of the trapezium, which corresponded to the radial residual bone distances after positioning of the cup.
Résultats : Differences between the both radial residual bone distances were assessed using Student's t-test. The width of the trapezius had a significantly higher mean value than the distal articular surface of the trapezius (p < 0.01), and their midpoints did not match. Thus, after positioning the simulated 9 mm diameter of the prosthetic cup, centered on each midpoints, the radial residual bone distance was up to 33% greater using the width of the trapezoid (p < 0.01).
Discussion : Our study suggests that the middle of the trapezium width is the most reliable radiographic landmark for centering the trapezial prothetic cup in the total joint arthroplasty by preserving better bone stock on the radial side without depleting the ulnary side, thus reducing the risk of cup loosening.
Hand motion analysis of functional tasks – repeatability and marker visibility
G. Fischer1, L. Reissner1, R. List1, D. Jermann1, M. Calcagni1 (1Zürich)
Show text
Objective: The aim of this study was to demonstrate the feasibility of simultaneously measuring all finger joints, the wrist and the radio-ulnar joint during daily activities using a 3D motion capture system. Main interest was in verifying good marker visibility and quantifying repeatability of angular motion patterns during functional tasks.
Method: Twenty healthy volunteers were recorded with a motion capture system during eight functional activities: opening a jar, a bottle and yoghurt, writing, typing, lifting a 1kg, 3kg and a small object. 46 skin markers were used to collect kinematic data of the hand, forearm, thumb and fingers simultaneously. Each task was repeated five times.
The visibility of the markers was reported as a percentage over the entire duration of the task. The intra- and inter-subject standard deviation (SD) between the angle curves was used as a measure of repeatability.
Results: Overall marker visibility was 97%, with markers for calculation of wrist, thumb and MCP kinematics achieving high visibility of over 99%, elbow and PIP >95% and DIP only 88.5%.
The averaged intra- and inter-subject SD over all tasks and joints was 4.9° and 10.2° respectively.
Conclusion: Overall, good data quality was achieved, thus confirming the feasibility of assessing hand kinematics during daily activities. However, in some tasks visibility of the markers for DIP3-5 joints was limited.
The movements were repeatable within a subject, but relatively large inter-individual differences were found. The tasks varied regarding repeatability, e.g. writing was the most repeatable activity within subjects (3.2°), but large differences between subjects were found for this task (11.7°). Using a heavier dumbbell weight (3kg vs. 1 kg) increased the repeatability of finger kinematics. Future studies should investigate the impact of the load on repeatability.
The angular motion patterns of healthy volunteers showed a relatively large inter-subject normal range. With the aim of quantitatively measuring hand function, future studies will investigate whether and to what extent patients' movement patterns and functional constraints can be distinguished from these normal values.
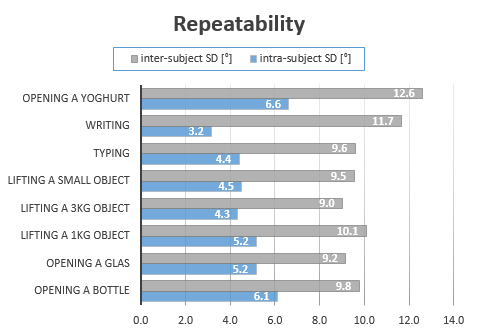
Inter- and intra-subject repeatability.png -
09:30 – 10:30
Gartensaal 2
Communications libres I
P. Chèvre, Bern (CH) / E. Marthaler, Biel (CH)COVID et comment un cours de thérapie de la main a quand même eu lieu au Sri Lanka !
B. Loos1, S. Ewald1 (1Zürich)
Show text
Introduction
Un cours de thérapie de la main déjà planifié pour des thérapeutes au Sri Lanka ne peut avoir lieu à cause de la pandémie de coronavirus – que faire ? L’annuler ou y a-t-il des alternatives ? Pour autant que les participants au Sri Lanka aient accès à Internet, il devrait être possible d’enseigner les bases de la thérapie de la main en ligne. Après concertation avec notre partenaire local au Sri Lanka, nous avons considéré cela comme un nouveau défi.
Méthode
Un questionnaire en ligne transmis aux thérapeutes intéressés au Sri Lanka nous a donné un aperçu de leur niveau de connaissance. La formation continue a finalement eu lieu avec 24 participants via Zoom et contenait six sessions en ligne de deux heures chacune réparties sur 3.5 mois.
Les cours ont été dispensés au moyen de présentations PowerPoint, de tables rondes, de séquences vidéo et d’exercices pratiques. Entre deux sessions d’enseignement, les participants ont été invités à travailler en groupe sur des devoirs et à les soumettre. Un learning center en ligne a été créé sur la plateforme groupspaces.com pour ce cours.
Objectifs
A la fin du cours :
- Les participants ont des connaissances de base en rééducation de la main.
- Une sélection de fiches d’évaluation et de feuilles d’information pour le patient qu’ils ont eux-mêmes créées et qui sont utiles pour la pratique clinique quotidienne au Sri Lanka est à disposition des participants.
- Un réseau s’est formé entre les thérapeutes et l’échange de connaissances et la collaboration sont encouragés.
Conclusion
Nous avons constaté que le cours en ligne avec des séquences d’enseignement échelonnées présente des avantages par rapport à l’enseignement en bloc. Les participants ont eu le temps d’assimiler la matière apprise et d’acquérir une première expérience pratique, tout en rendant des devoirs pertinents pour leur travail quotidien. En tant qu’instructrices, grâce aux travaux, nous avons pu nous faire une idée du niveau de connaissance ainsi que de la manière d’appliquer ces nouvelles notions. Par conséquent, il a été possible d’adapter en permanence le contenu du cours et nos stratégies d’enseignement. Nous avons pu observer l’effet de l’apprentissage. Les réactions positives des participants nous ont encouragées et confirmé qu’un cours de rééducation de la main peut être mis en place en ligne de manière efficace.
En 2021, le groupe de participants a été élargi au Bangladesh et le cours en ligne a été dispensé par des intervenants de cinq pays.
Un cours de rééducation de la main en ligne est abordable pour tous les acteurs, respectueux de l’environnement, favorise le développement de la thérapie de la main au niveau local et peut avoir lieu malgré une pandémie.
Behaviour Change?* Anciennes et nouvelles preuves illustrées par un exemple de cas
B. Aegler1, C. Wildhaber-Phillips1 (1Zürich)
Show text
Les patients souffrant d’une blessure ou d’une pathologie à la main passent par plusieurs changements de comportement pour une rééducation réussie. Dans la phase aigüe, il s’agit la plupart du temps d’apprendre à faire les activités en épargnant la main blessée, puis la phase de réadaptation consiste à lentement réintégrer et réentraîner la main concernée dans les activités quotidiennes et professionnelles. Comment les thérapeutes peuvent-ils soutenir leurs patients de manière optimale durant ce processus ?
Ces changements de comportement ont été décrits dans les années 80 à travers le modèle transthéorique du changement (MTT) expliquant les six phrases du changement de comportement. Schwarzer développa un peu plus tard l’approche du processus d’action de santé (APAS)** qui se concentre sur la distinction entre intention et comportement (Intention-Behaviour-Gap). Les deux modèles soutiennent que le défi est de surmonter le passage de l’intention à l’action. Des approches récentes comme « Tiny Habits » de BJ Fogg 2019 s’appuient également de plus en plus sur la recherche neuroendocrinienne. Divers moyens aidant à surmonter ce passage seront présentés ici, comme le déclenchement ciblé d’hormones qui permet plus facilement des changements de comportement au quotidien. Cette présentation montrera les points forts de ces différents modèles ainsi que les dernières connaissances biologiques de la recherche sur les hormones, sur lesquelles « Tiny Habits » se base, et un exemple de cas (violoniste) sera utilisé pour illustrer la mise en œuvre possible en thérapie.
Références :
- Prochaska, J. O. & DiClemente, C. C. (1982). Transtheoretical therapy: Toward a more integrative model of therapy. Psychotherapy: Theory, Research, and Practice, 19, 267-288
- Schwarzer, R. (1992). Self-efficacy in the adoption and maintenance of health behaviors: Theoretical approaches and a new model. In R. Schwarzer (Ed.), Self-efficacy: Thought control of action (pp. 217-243). Washington, DC: Hemisphere.
- Fogg B.J. (2020) Tiny Habits: The Small Changes That Change Everything Virgin Books London
Notes de la traductrice :* Changement de comportement
** En anglais dans le texte : Health Action Process Model (HAPA)« Vous et moi » – ensemble, nous traitons la main ; la relation thérapeutique en rééducation de la main
A. Schmid1 (1Thun)
Show text
Nous voulons tous que le patient ne reparte pas comme il est arrivé, pas après une séance de thérapie et encore moins à la fin de la rééducation. Patient et thérapeute souhaitent tous deux la meilleure récupération fonctionnelle possible de la main – nous nous engageons dans une voie très importante et efficace à travers une bonne collaboration. La question de la meilleure thérapie possible, la plus efficiente qui soit, nous accompagne constamment. Quels facteurs influencent le changement ?
Lambert (1999) a étudié en psychothérapie les facteurs entraînant le changement chez les patients. La découverte récente de ce modèle m’a inspirée et motivée à en savoir plus. Même si la relation thérapeutique en rééducation de la main est un peu inférieure aux 40% décrits par Lambert, elle a pourtant une grande importance dans ce domaine.
Taylor et al. (2009) ont réalisé un questionnaire randomisé auprès d’ergothérapeutes américains sur l’auto-efficacité « Use of Self », c’est-à-dire les habitudes/attitudes et les expériences en matière de relation thérapeutique. Plus de 80% des thérapeutes pensent que l’intervention thérapeutique propre à l’individu est le moyen le plus important pour les résultats de la thérapie. Par conséquent, le raisonnement clinique devrait toujours impliquer la personne concernée. La plupart des thérapeutes déclarent avoir souvent à toujours des sentiments positifs envers leurs patients – ce qui est une condition idéale pour une thérapie réussie. Toutefois, la plupart des thérapeutes estiment ne pas être assez formés et ne pas disposer des connaissances suffisantes.
A maintes reprises, des patients nous ont contactés après des années et ont souhaité suivre une nouvelle thérapie avec leur ancien thérapeute. Parfois, ils ont reçu les recommandations personnelles d’une amie. Il est important pour eux de savoir qui s’occupe d’eux.
C’est un exemple pratique parmi tant d’autres montrant l’importance de la relation thérapeutique au quotidien.
En me basant sur des résultats d’études et par l’intermédiaire d’expériences dans la pratique, j’aimerais, avec les participants au congrès, porter l’attention et l’enthousiasme non seulement sur la main, mais surtout sur l’humain et la relation thérapeutique.
Taylor, R. R., et al. (2009). "Therapeutic use of self: a nationwide survey of practitioners' attitudes and experiences." Am J Occup Ther 63(2): 198-207.
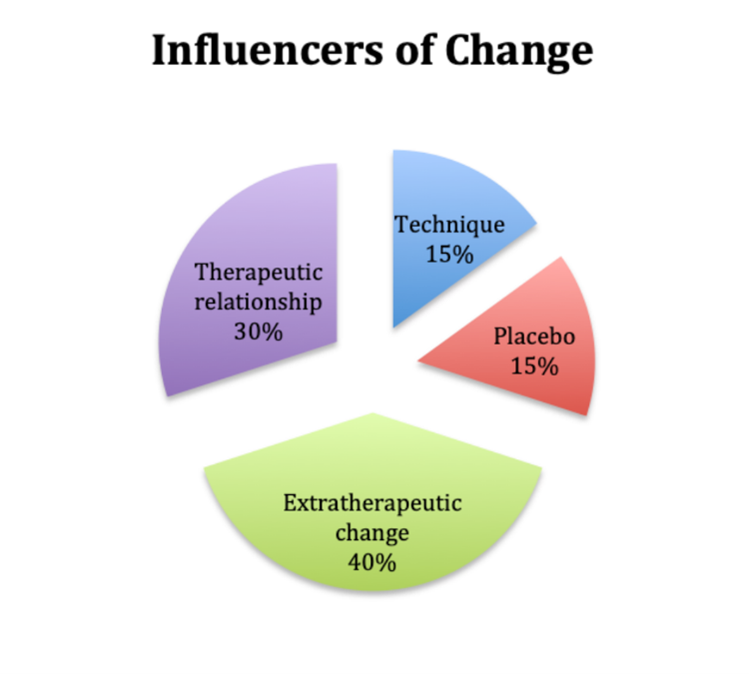
Grafik influencers of Change.png -
09:30 – 10:30
Vortragssaal 2
Communications libres I B
Bones
A. Schweizer, Zürich (CH) / M. Häfeli, Chur (CH)The spanning plate as an internal fixator in distal radius fractures – a prospective cohort study
R. Liechti1, R. Babst1, U. Hug1, B. C. Link1, B. van de Wall1, M. Knobe1, F. Beeres1 (1Luzern)
Show text
Objective
Minimal invasive temporary spanning plate (SP) fixation of the wrist has been described as an alternative treatment method in complex distal radius fractures (DRFs). The purpose of this study is to conduct an outcome analysis of all consecutive DRFs treated by SP fixation at a level I trauma centre in central Switzerland.
Patients and Methods
All consecutive patients undergoing SP fixation of DRFs were prospectively included in a single level I trauma centre between 01/01/2018 and 31/12/2020. Indication for SP fixation included DRFs with severe metaphyseal comminution, radiocarpal fracture dislocations with concomitant ligamentous injuries and very distal intra-articular fractures lacking the possibility of adequate plate anchoring. Post-operative assessments included radiological, functional, and patient-rated outcomes at a minimum of 12 months follow-up.
Results
In the mentioned timeframe, a total of 508 DRFs were treated operatively of which 28 underwent SP fixation. Average age was 58.1 years (range 22-95 years). The fracture type ranged from AO/OTA type B1.1 to C3.3 and included 8 fracture dislocations. The mean follow-up time was 14.5 months (range 12-24 months). SP removal was performed on average 3.7 months after the initial operation (range 1.4-6.5 months). Radiological evidence of fracture healing appeared on average 9.9 weeks (range 5-28 weeks) after the initial operation. One patient experienced oligosymptomatic non-union. Complications included 2 patients with tendon rupture and one patient with extensor tendon adhesions needing tenolysis at the time of plate removal leaving an overall complication rate of 12%. There was no implant failure and no infection. Mean satisfaction score was 8 (range 0-10) and mean visual analogue scale for resting pain was 0.9 (range 0-9). The mean PRWE score was 17.9 (range 0-59.5) and the mean DASH score was 16.6 (range 0-60.8). Grip strength averaged 23kg (range 4-74kg) amounting to 68% of the opposite side. Mean radial inclination, volar tilt and ulnar variance at 1 year were all within the acceptable limit predictive of symptomatic malunion.
Conclusion
The radiological, functional and patient-rated outcomes in this study are remarkably good considering the complexity of the included fractures. Therefore, this method represents a valuable bail out treatment option for complex DRFs in selected patients.
Total wrist Implant in complex distal radius fractures in the elderly
I. Tami1, C. Mesoraca2, T. Giesen1 (1Gravesano; 2Neuchatel)
Show text
Introduction: Complex distal radius fractures with severe comminution and dislocation, reppesent a challenge for the hand surgeon, especially in the elderly. An osteoporotic bone on top, might be a critical factor influencing the stability of the fixation, often leading to questionable results. We present our primary experience with the immediate implantation of Motec total wrist implant in severely comminuted and displaced distal radius fractures in the elderly.
Materials and Methods:
From January 2020 to February 2021 we treated 7 distal radius fractures with a Motec total wrist implant. All patients were female with an average age of 79 years old (range 75-89). All sustained a distal radius fractures classified as C2 or C3. One patients had a fracture classified as C2 but with a large depressed and damaged area to the radius cartilage. There were 5 right wrist and 2 left. All patients were active and independent with no major health problem. One patient was diabetic.
Results: At 6 months follow up ( range 3-12) all patients recovered well. Prono-supination was substantially maintained and painfree in all cases. Average wrist extension was 42° (range 35°-60°) while average flexion was 50° ( 40°-70°). Jamar in position 2 gave an average strength of 78% of the controlateral wrist ( range 62%-85%). VAS was 1 (range 0-3) at rest. VAS under wrist load was 2 ( range 1-4). Maximum load observed was of 5 Kilograms. No major complications were observed. On patient required 4 months to fully recover wrist extension. In general wrist extension was the most difficult movement to recover.
Conclusion: As already largely accepted for other joints in the body, difficult fracture of the distal radius might benefit from an immediate total joint arthroplasty. The Motec implant seems to offer a reliable solution. Further studies and longer follow up might be required to better define indications.
DISCLOSURE: No financial conflict of interest to disclose
Surgical Fixation Techniques in Four-Corner Fusion of the Wrist: A Systematic Review of 1103 Cases
O. Andronic1, R. Labèr1, P. Kriechling1, D. Karczewski2, A. Flury1, L. Nagy1, A. Schweizer1 (1Zürich; 2Berlin DE)
Show text
Background: Four corner fusion (4CF) is a known treatment option for degenerative wrist conditions. Different techniques may be used and there is no general consensus on best implant. As such, it was the purpose of the current systematic review to compare fusion rates and outcomes depending on the fixation technique.
Methods: The systematic review was registered in the international prospective register of systematic reviews (PROSPERO): CRD42020164301. It followed the PRISMA guidelines. Original articles were screened using the following databases: CENTRAL (Cochrane Central Register of Controlled Trials), MEDLINE, EMBASE and Web of Science Core Collection. Studies reporting on outcome for four-corner fusion surgery were included. Studies with a minimum Level IV of evidence were considered eligible. Quality assessment was performed using the MINORS (Methodological Index for Non-Randomized Studies) criteria.
Results: 29 studies met the inclusion criteria, for a total of 1103 wrists. The mean age was 41.8 years (range 19-83). Mean follow-up overall was 43.5 months (range 24-146 months). Fusion weighted rates of 97% for K-wires, 94% for locking plates and 98% for non-locking plates. Reoperations occurred in 135 (12%) of all 1103 cases. Least reoperations occurred using K-wire fixation (10.4%) as opposed to locking plates (14.2%) or non-locking plates (11.7%).
Conclusion: Satisfactory fusion rates can be achieved independent of the fixation technique used in 4-corner arthrodesis. In terms of reoperations, K-wires showed an overall lower reoperation rate compared to other techniques.
Clinical, Radiological and Patient-Rated Outcome Comparison between Partial and Total Ulnar Head Implants
L. Estermann1, L. Reissner1, A. Schweizer1, L. Nagy1 (1Zürich)
Show text
Introduction: Painlessness, motion and joint stability are crucial for a well-functioning distal radioulnar joint. The same requirements apply to the ulnar head prosthesis. The aim of this study was to analyse the clinical and radiological outcomes after ulnar head replacement and to compare partial and total ulnar head implants.
Material and Methods: 22 patients with 23 implants were available with a mean follow up time of 7 years after distal radioulnar joint arthroplasty. Patient-rated outcome measures by visual analog scale, PRWE and DASH questionnaire, range of motion measurements, radiographic examination and grip strength as well as pronation and supination torque were assessed. Additionally, sonography was performed to quantify the instability of distal radioulnar joint.
Results: Patients showed a low level of pain at rest and under load, a median DASH score and PRWE of 12 after implantation of a partial ulnar head prothesis, 20 and 22 after implantation of a total ulnar head prosthesis, respectively. While the range of motion in patients with partial ulnar head implants was slightly reduced in comparison to the preoperative condition and to the patients with total ulnar head implants, there was a tendency to a higher grip strength as well as supination and pronation torque. Both types of prosthesis showed sigmoid notch resorptions and resorptions around the neck. The sonographically assessed instability of the distal radioulnar joint did not show any significant differences between the prostheses.
3D planned reconstruction of the distal radioulnar joint congruency of severe ulna minus variance
L. Reissner1, L. Estermann1, A. Schweizer1 (1Zürich)
Show text
Introduction:
Dysplasia of the distal radioulnar joint (DRUJ) and posttraumatic conditions may lead to symptomatic ulna minus variance. Until now, there is no evidence for treatment of ulnar dysplasia Swanson Grade I. By recent developments in computer-assisted surgery, the use of patient-specific instruments (PSI) has been described as a reliable method to accurately correct even complex malunions of the forearm. With a 3D planned radius corrective osteotomy a better DRUJ congruency could be achieved. The primary objective of this study is to describe our treatment approach to restore a congruent DRUJ. Furthermore, we analyzed postoperative pain, hand function, range of motion and grip strength.
Method:
All patients with a severe ulna minus who received a PSI guided osteotomy of the radius with a minimal follow up of 6 months were included. Based on three-dimensional computed tomography imaging data PSI were planned and produced to guide the osteotomy and further osteosynthesis. Subjective assessment was based on a visual analogue scale (VAS) for pain, DASH and PRWE score. Range of motion (ROM) and grip strength data were extracted from the documentation of the last follow up examination. Ulna variance values were measured by means of the method of perpendiculars.
Results:
10 patients with a mean age of 23 years received corrective osteotomies of the radius in order to address their ulna minus variance. The follow up examination took place on average 3.1 years after surgery (range 9 months - 5.7 years). On the VAS scale, the pain was 0 without load in five patients and 2-4 in the other five patients. In addition, DASH score was 24 and PRWE score 30. The mean active ROM of pronation and supination was 78/0/84° preoperative and 75/0/82° postoperative. The grip strength increased from mean 24 kg preoperative to 34 kg postoperative. The mean ulna variance was before surgery minus 6.2 mm (SD 2.7) and postoperative minus 0.5mm (SD 0.6).
Conclusion:
Our technique, based on 3D bone modelling and application of PSI, permitted to perform a precise osteotomy, that would have otherwise been difficult to treat using any of the few procedures described in the literature to date. Most patients showed nearly unchanged range of motion and an improved grip strength postoperative with no or moderate pain during rest and activity. We recommend 3D planned radius corrective osteotomy as an approach to manage symptomatic ulna minus variance.
Morphometrie der distalen Ulna im Hinblick auf das Prothesendesign
P. Furrer1, L. Nagy1, A. Schweizer1, L. Reissner1 (1Zürich)
Show text
Soll bei der prothetischen Versorgung des distalen Radio-Ulnar-Gelenkes (DRUG) lediglich der Ulnakopf im Sinne einer Ulnakopf-Hemiprothese (UKHP) ersetzt werden, sollte das Implantat die ursprüngliche Anatomie weitestmöglich reproduzieren. Hierfür haben wir die, für das Design einer UKHP relevante Geometrie der distalen Ulna untersucht.
40 Computertomogramme von gesunden Ulnae wurden segmentiert und in einem 3-D Programm bearbeitet: 4 Chirurgen haben in die distalen 7 cm der Markhöhle einen in der Grösse angepassten Zylinder, analog einem Prothesenschaft, eingepasst. Ein zweiter grössenvariabler paralleler Zylinder wurde um den gelenkbildenden Teil des Ulnakopfes angelegt. Gemessen wurden die Radii der beiden Zylinder sowie der Versatz der beiden Zylinderachsen bezüglich Abstand und Richtung.
Der Radius der distalen Markhöhle betrug im Mittel (SD): 7.92mm (0.74); des Ulnakopfes: 2.89mm (0.42). Der Abstand der beiden Zylinderachsen war: 3.89mm (0.78); die Richtung des Offset: 8.63° Supination (15.28). Die Messungen der genannten Variablen waren sehr konsistent mit einer Interrater-Reliabilität von 0.93; 0.88; 0.82 und 0.90. Die Grössen der beiden Zylinder korrelierten statistisch signifikant zu 0.622 (Pearson).
Eine möglichst anatomiegetreue UKHP sollte einen wesentlichen Versatz zwischen der Prothesen-Schaft-Achse und dem Prothesen-Kopf aufweisen. Dies dürfte eine Voraussetzung darstellen für die korrekte Spannung der ligamentären Stabilisatoren des DRUG: Der diversen Anteile der membrana interossea und im Fall einer partiellen Hemiprothese auch des belassenen TFC. Dies ist bei den erhältlichen UKHP’s nicht der Fall und womöglich die Ursache der häufigsten Komplikation – der DRUG-Instabilität.
SUPEXOR: implementing the ICHOM Hand and Wrist Conditions set in Switzerland
M. Calcagni1, M. E. Gunning1 (1Zürich)
Show text
Introduction
One of the biggest challenges of modern health systems is to truly put patients first. That requires measuring performance, listening to patients’ opinions and improving outcome and patients’ experience. In Switzerland there is no system to register outcomes measurements of treatments for hand and wrist conditions. Outcome measurements can control and improve treatment quality, catalyze communication and decision making between physicians and patients and build a research database, to be used for comparative research, health technology assessment and benchmarking between institutions.
Aim of this project is to establish an outcomes registry in a pilot group of Swiss hand surgery institutions and to set the basis for a potential upscale at national level.
Methods
In 2020-2021, four Swiss hospitals built an outcomes registry based on existing software of Dutch medical engineers, using the newly developed Standard set for hand and wrist conditions by the International Consortium for Health Outcomes Measurement. Patients are risk stratified and divided over five tracks according to the type of problem to allow for optimal analysis. Treatment outcomes of hand and wrist conditions are entered by surgeons, therapists and patients in a multi-language registry to serve the needs of all stakeholders.
Results
The registry went live in the last quarter of 2020 and over 300 patients have been registered so far. It is too early to evaluate results and measure impact on patient care, but the first experience is positive. Semi-automatic track assignment and automatic emails are features that reduce clinician’s burden. Patient’s compliance has been growing during the first months of clinical use of the registry.
Conclusion
Establishing a quality registry is a big endeavor with risks and pitfalls, but with careful planning and a professional team it can be mastered successfully. The most important and challenging, is to convince and motivate physicians to engage in this project, not seeing it as a threat, but rather as an opportunity for improvement. Quality control, pay per performance and benchmarking are becoming reality and for physicians it is fundamental to stay on the cutting edge of these developments, keep the lead and advocate for themselves and their patients. Quality can only be improved if it is measured in a meaningful manner. In an outcomes registry, data are collected in a structured way, building value for all stakeholders involved.
-
10:30 – 11:00
Pause café
-
11:00 – 11:15
Gartensaal 1 A-C
Report Forschungsfonds
M. Calcagni, Zürich (CH)Ultrasound in carpal tunnel syndrome: the inlet and outlet ratio
S. Hirsiger, Bern (CH)
-
11:00 – 12:30
Gartensaal 2
Communications libres II
B. Tobler, Bern (CH) / J. Busskamp, Basel (CH)Programme d’exercices à domicile par vidéo en rééducation de la main – un pas vers le futur
D. Kuster1, K. de Cillia2 (1Zürich; 2Altstätten)
Show text
Les programmes d’exercices à domicile sont une composante essentielle pour la réussite d’un traitement en thérapie de la main et leur instruction est une tâche importante du thérapeute. Différents facteurs tels que les problèmes de compréhension ou un soutien insuffisant au patient peuvent compliquer le processus.
Les progrès technologiques et les changements sociétaux actuels ouvrent de nouvelles possibilités. Dans le domaine de la santé, nous sommes également de plus en plus souvent confrontés aux nouvelles technologies. Le support de la vidéo est fréquemment abordé dans la littérature. En thérapie de la main, un grand potentiel est attribué à l’utilisation de l’enseignement par vidéo pour les programmes d’exercices à domicile1.
En tant que thérapeutes de la main, nous nous sommes intéressées au potentiel d’optimisation du processus d’instruction des programmes d’exercices à domicile. Nos recherches Internet pour trouver des consignes vidéo appropriées et conformes à nos exigences sont restées infructueuses. Il existe peu de vidéo d’instruction produites par des thérapeutes de la main expérimentés2.
Dans le cadre du CAS en thérapie de la main, nous avons élaboré un guideline fondé sur la littérature afin de créer un programme d’exercices à domicile sur vidéo. Par cet intermédiaire, nous avons produit six vidéos contenant divers exercices et les avons utilisées dans la pratique. Ce processus nous a permis d’acquérir une expérience précieuse dans le domaine de la vidéo. Les réactions des patients et des membres de l’équipe, ainsi que nos propres constatations, ont stimulé notre réflexion sur la nature et le contenu de l’enseignement. Par conséquent, nous avons adapté notre production et conçu une autre vidéo, plus complète.
Nous aimerions, lors de notre présentation à l’auditoire, mettre en lumière l’utilisation de consignes vidéo en thérapie de la main et relater notre expérience à ce propos. Nous sommes persuadées que les instructions vidéo pour les programmes d’exercices à domicile seront une facilitation dans la pratique quotidienne future.
1 Ouegnin, A. & Valdes, K. (2019). Client preferences and perceptions regarding a written home exercise program or video self-modeling: A cross-sectional study. Journal of Hand Therapy. Published online January 21, 2019. DOI: https://doi.org/10.1016/j.jht.2018.09.006.
2 Villafañe, J. H., Cantero-Tellez, R., Valdes, K., Usuelli, F. G. & Berjano, P. (2018). Educational Quality of YouTube Videos in Thumb Exercises for Carpometacarpal Osteoarthritis: A Search on Current Practice. Hand, 13(6), 715-719.
Home exercise program modalities in carpal tunnel release rehabilitation: handout or smartphone?
P. Lorenzo1, S. Rosana2, F. Gaetano1, I. Tami3 (1Mendrisio; 2Giubiasco; 3Gravesano)
Show text
Background
It is common practice to recommend home exercise program after carpal tunnel release surgery. Usually, these exercises have been delivered in the way of written handouts with pictures. However, the possibilities offered by the use of the smartphones, can be valuable for both, therapists and patients. It is outstanding to discover the best modality, to maximise patient’s compliance in order to ensure the best outcome. The aim of this study is to investigate the patients’ preference between written handouts with pictures and videos recorded using their smartphone.
Methods
A cross-sectional study is conducted on patients who access at the rehabilitation facility after carpal tunnel release surgery. The day after surgery patients receive the written handout plus the instructions to record the same exercises using their personal smartphone. The patient is asked to perform the exercises one day in accordance to the written instructions and the day after by watching the videos recorded by themselves the first day. Concluded 10 days of program, a satisfaction evaluation form is delivered. No validated instruments have been found in the peer reviewed literature, therefore, it is necessary to create a standardized assessment tool. Regarding the evaluation scale set-up, the principles of customer satisfaction is used, especially the “Servqual” approach. The following domains are investigated: usefulness, comprehensibility, feasibility and motivation.
Discussion
The study is in progress with the currently inclusion of 25 patients. The data collection is expected by the end of August 2021 with the total enrolment of 30 patients. The data will be processed to find out which of the two modalities scored the highest value on the 4 items. It will then be possible to cross demographic data with preferences. Preliminary data shows that the smartphone application can be valuable in increasing adherence to the home exercise program.
References
Ouegnin A, Valdes K. Client preferences and perceptions regarding a written home exercise program or video self-modeling: A cross-sectional study. J Hand Ther. Jan-Mar 2020;33(1):67-72.
Cole T, Robinson L, Romero L, O’Brien L. Effectiveness of interventions to improve therapy adherence in people with upper limb conditions: A systematic review. J Hand Ther. Apr-Jun 2019;32(2):175-183.
Asuboteng P, McCleary K, Swan J. SERVQUAL revisited : a critical review of service quality. Journal Of Services Marketing. Dec 1996;10(6):62-81.
La mobilisation neurodynamique comme programme d’exercices à domicile
E. Vola1, F. Flütsch1 (1Chur)
Show text
Nous avons constaté que les instructions de mobilisation neuroméningée étaient données différemment dans notre équipe et que nos fiches de programme d’exercices à domicile pour les patients n’incluaient aucun degré de difficulté. Dans le cadre de notre travail de CAS, nous avons révisé ces fiches dans le but d’avoir des exercices progressifs pour le nerf médian, le nerf ulnaire ainsi que le nerf radial. En outre, nous souhaitions former l’équipe afin que chacun enseigne les exercices de manière uniforme.
En nous basant sur la littérature et l’anatomie, nous avons déterminé la manière dont les différents nerfs glissent, les mouvements durant lesquels ils sont mis en tension et ceux durant lesquels ils sont relâchés. De plus, nous voulions savoir à quel moment ces exercices sont recommandés et quelles sont leurs contre-indications.
Les exercices consistent en glissement et mise en tension. Les premiers engendrent des mouvements de glissement du nerf par rapport aux tissus environnants, sans créer beaucoup de tension ou de compression (Shacklock, 2008). Lors des seconds, les articulations sont positionnées de telle manière à ce que la tension du nerf se fasse de manière croissante.
Lohkamp et al. (2018) recommandent de commencer les exercices le plus loin de la zone affectée, allant d’un glissement bilatéral vers un glissement unilatéral, puis d’une mise en tension unilatérale vers une mise en tension bilatérale.
En raison des innombrables possibilités d’exercices, nous avons opté pour une représentation schématique. Une fiche a été créée pour chacun des trois nerfs – médian, ulnaire et radial – en décrivant l’intensité croissante des exercices. Nous avons conçu une fiche pour les mises en tension sur laquelle les exercices de mobilisation peuvent être sélectionnés en fonction du problème rencontré.
Bibliographie :
Lohkamp, M., Small, K., & Herrington, L. (2018). Neurodynamik (1. Aufl.). München: Elsevier.
Shacklock, M. (2008). Angewandte Neurodynamik (1. Aufl.). München: Elsevier.
Die patientenspezifische Funktionsskala (PSFS)* – une évaluation précieuse pour la rééducation de la main
M. von Haller1 (1Zürich)
Show text
Introduction : La prise en compte du point de vue du patient est une composante importante de l’évaluation et du traitement centrés sur le client (1). L'échelle fonctionnelle spécifique au patient (PSFS) recueille les limitations fonctionnelles individuelles sur la base d’activités définies par le patient (2).
Objectif : Évaluation des propriétés psychométriques de la PSFS chez des patients en rééducation de la main et démonstration des possibilités d’utilisation de la PSFS en thérapie de la main.
Méthode : Recherche de littérature systématique dans les bases de données médicales et études de cas issus de la pratique.
Résultats : Dans les neuf études incluses, la PSFS montre une bonne fiabilité, validité et sensibilité au changement chez les patients souffrant d’une blessure ou d’une pathologie du membre supérieur, comme par exemple la maladie de Dupuytren ou une lésion nerveuse périphérique (3-5). Il s’agit d’un instrument centré sur le client, facile d’utilisation et peu chronophage, pouvant également être utilisé pour fixer des objectifs individuels et un plan de traitement (6).
Discussion : Malgré de bonnes propriétés psychométriques, davantage de preuves sont nécessaires pour l’utilisation de la PSFS en rééducation de la main, notamment en ce qui concerne les diagnostics particuliers et leur intégration dans la recherche.
Note de la traductrice :
*L’échelle fonctionnelle spécifique au patient
Bren L. The importance of patient-reported outcomes... it’s all about the patients. FDA Consumer. 2006 Dec 11;40(6):26–32.
Stratford P, Gill C, Westaway M, Binkley J. Assessing Disability and Change on Individual Patients: A Report of a Patient Specific Measure. Physiotherapy Canada. 1995 Oct;47(4):258–63.
Rosengren J, Brodin N. Validity and reliability of the Swedish version of the Patient Specific Functional Scale in patients treated surgically for carpometacarpal joint osteoarthritis. Journal of Hand Therapy. 2013 Jan;26(1):53–61.
van Kooij YE, Poelstra R, Porsius JT, Slijper HP, Warwick D, Selles RW. Content validity and responsiveness of the Patient-Specific Functional Scale in patients with Dupuytren’s disease. Journal of Hand Therapy. 2020 Apr;S0894113020300405.
Wright HH, O’Brien V, Valdes K, Koczan B, MacDermid J, Moore E, et al. Relationship of the Patient-Specific Functional Scale to commonly used clinical measures in hand osteoarthritis. Journal of Hand Therapy. 2017 Oct;30(4):538–45.
Jolles BM, Buchbinder R, Beaton DE. A study compared nine patient-specific indices for musculoskeletal disorders. Journal of Clinical Epidemiology. 2005 Aug;58(8):791–801.
Une base de données sur les tendons fléchisseurs – suivi d’un projet de recherche multicentrique
V. Beckmann-Fries1, L. Schrepfer2, L. Hemelaers2, E. Oberfeld3, M. Calcagni1, B. Tobler-Ammann3 (1Zürich; 2Basel; 3Bern)
Show text
Introduction : En 2013, les services de thérapie de la main de trois hôpitaux universitaires ont eu une réunion sur la prise en charge des tendons fléchisseurs, ce qui a été l’élément déclencheur pour la création d’un protocole de traitement commun. Ce fût le début d’une collaboration intensive ayant pour but de recueillir, documenter et analyser de manière standardisée les résultats de traitement après une telle lésion.
Objectif : Grâce à la collaboration de ces trois grandes cliniques, un nombre suffisamment grand de données sur les tendons fléchisseurs sera obtenu dans un temps relativement court afin de faire un bilan des résultats de traitement ainsi que des adaptations appropriées pour l’élaboration du protocole.
Méthode : Des mesures cliniques sont effectuées à des moments bien précis auprès des patients souffrant d’une lésion du tendon fléchisseur dans les trois services de thérapie de la main. Une base de données (REDCap) a été installée pour la collecte conjointe des données. Cela permet à toutes les cliniques, indépendamment de leur emplacement, d’avoir accès aux données à tout moment.
Résultats : Cette étude a débuté en 2014 et sera poursuivie jusqu’en 2025. Actuellement, les données de 308 patients atteints de 343 doigts longs et pouces blessés sont contenues dans la banque de données. Celle-ci inclut 202 hommes (65.6%) et la moyenne d’âge des patients est de 36.6 ans (SD 13.6). Dans la majorité des cas, la blessure se situe en zone 2 (n=205), suivie de la zone 1 (n=90) et de la zone 3 (n=48). Dans 56.0% (n=192) des doigts longs et pouces blessés, un nerf digital a également été traité chirurgicalement. 96.1% (n=296) des patients ont bénéficié d’une attelle dorsale longue, 3.9% (n=12) ont porté une attelle « Manchester Short Splint ». Sans complication particulière (pas de rupture, de CRPS ou de ténolyse), la rééducation de la main a duré en moyenne 19.1 semaines (SD 9.3). La durée du traitement était de 23.3 semaines (SD 13.2) en cas de ténolyse ultérieure et de 29.7 semaines (SD 10.0) en cas de CRPS concomitant.
Pertinence pratique : Il est important de recueillir des mesures suite à une blessure ou à une maladie touchant la main de manière standardisée et à des moments bien définis (Selles et al. 2020). Cela permet un contrôle de haute qualité des résultats de traitement, fournit la base pour l’amélioration de ce dernier et est l’occasion d’un échange ciblé sur le sujet.
Selles RW, Wouters RM, Poelstra R, et al. Routine Health Outcome Measurement: Development, Design, and Implementation of the Hand and Wrist Cohort. Plast Reconstr Surg. 2020;146(2):343-354.
The Consensus Wrist Index (CWI), an Outcome Tool for Interdisciplinary Use
S. G. Ewald1, E. Vögelin2, R. Wollstein3 (1Zürich; 2Bern; 3New York US)
Show text
Introduction: The consensus wrist index (CWI) is an interdisciplinary outcomes visualization tool relevant for surgeons and therapists. It was developed following an interdisciplinary wrist outcome meeting in 2018. Following the second revision in 2019, it has been available to clinicians for use in practice.
Method / Aims: The CWI combines existing and established assessments to create an overall picture of the patient’s functional situation. It includes objective measurements: grip strength and range of motion, and patient-rated outcome measures: Patient-Specific Functional Scale (PSFS), Patient Rated Wrist and Hand Evaluation (PRWHE), the Single Answer Numeric Evaluation (SANE), and the work module of the Michigan Hand Questionnaire (MHQ). Following data collection, the data is input into an excel file. All data points are equally weighted and visualized on a spider diagram, which can accommodate 3 points in time. It takes about 10 minutes to input data into the Excel file and generate the resulting graphic. Case examples demonstrating the use of the tool in practice will be discussed.
Conclusion: The CWI is a new tool that can assist clinicians and patients in the visualization of multiple aspects of a wrist condition. The tool goes beyond objective measurements and incorporates patients’ specific priorities and needs to gain a comprehensive picture of the situation. It generates a visual representation of outcomes; this is advantageous as multiple domains are viewed in a single diagram. The CWI provides a foundation for discussing the status, progress, and possible further interventions with patients and other clinicians. It can be utilized, in patients with injuries that are treated conservatively to monitor progress, prior to surgery to measure pre- /post-surgical outcomes or following surgery to track progress. A feasibility study is underway, and we would welcome input from clinicians that have used the CWI in their clinical practice.
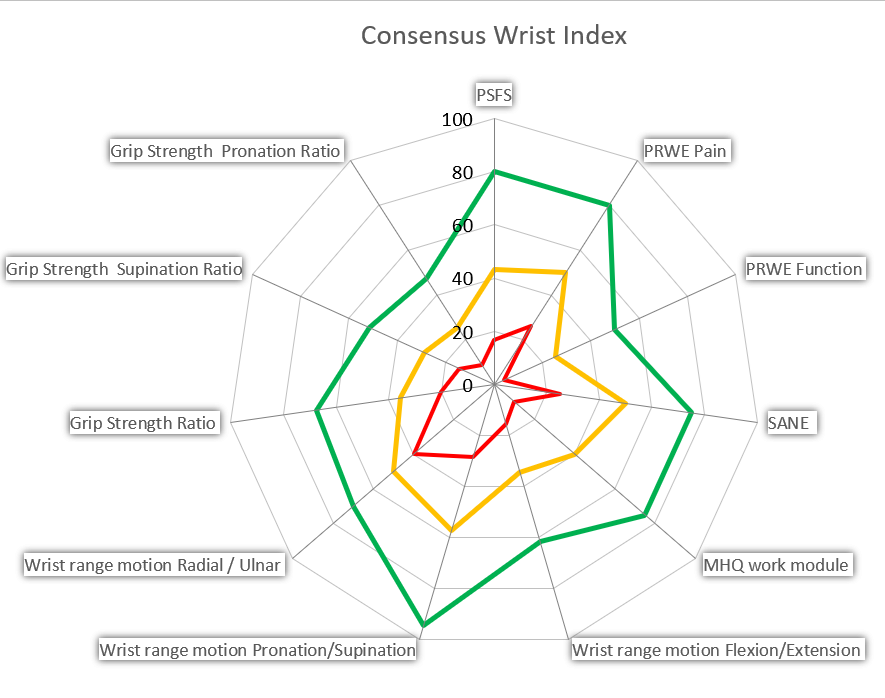
Example of CWI -
11:15 – 12:30
Gartensaal 1 A-C
Session principale I
In sport, everything revolves around the hand…
I. Tami, Gravesano-Lugano (CH) / T. Hauri, Zürich (CH)Introduction
I. Tami, Gravesano-Lugano (CH) / T. Hauri, Zürich (CH)
Managing athletes in fighting sports
L. Pegoli, Torino/Monza (IT)
Teamwork in managing athletes
G. Matera, Milano (IT)
Complex bilateral wrist injuries in mountain biker: case report
M. Lombardo, Torino/Monza (IT)
Resistance training in rehabilitation
S. Küng, Zürich (CH)
Discussion and take home message
L. Pegoli, Torino/Monza (IT) / I. Tami, Gravesano-Lugano (CH) / T. Hauri, Zürich (CH)
-
12:30 – 13:45
Lunch-buffet – rencontre dans l’exposition
-
12:45 – 13:30
Gartensaal 1 A-C
Symposium de midi 1
Diversität – eine handchirurgische Annäherung
Vernetzung im World Café
-
12:45 – 13:30
Gartensaal 2
Symposium de midi 2
NanoScope
Dr. med. Mischa Wiegand, Facharzt für Chirurgie FMH, Handchirurgie FMH
-
13:30 – 15:00
Vortragssaal 2
Atelier 1P. Kammermann, Bern (CH) / I. Cianci, Affoltern am Albis (CH)Attelle Sugar Tong pour une lésion du TFCC – notre modèle d’attelle
T. Hauri, Zürich (CH) / M. Löffel, Zürich (CH)
Mit freundlicher Unterstützung: 3M (Schweiz) GmbH, Rüschlikon / Orthopartner AG, Niederlenz
Show full description
Il existe différentes attelles pour le traitement des lésions du TFCC. Toutes ont pour but d’éviter ou de limiter la pronation et la supination de l’avant-bras. L’attelle « Sugar Tong » en est un exemple. Notre attelle « Sugar Tong » est légèrement modifiée et fabriquée en Scotchcast. L’attelle est bien tolérée par nos patients.
Durant notre atelier, nous donnerons un bref aperçu des diverses attelles pour le traitement du TFCC et nous présenterons notre modèle. Nous montrerons comment fabriquer cette attelle et nous guiderons les participants lors de la confection de leur propre attelle (voir image ci-dessous).

-
13:45 – 15:00
Gartensaal 1 A-C
Session principale II
Grasping across boundaries – recent advances in tetrahand surgery
S. Koch-Borner, Nottwil (CH) / S. Schibli, Nottwil (CH)Mobility and stability
J. Fridén, Nottwil (CH)
Muscle excitability – refined diagnostics
S. Koch-Borner, Nottwil (CH)
Grasp and release - advanced surgical options
S. Schibli, Nottwil (CH)
Motor relearning strategies
K. Schmuck, Nottwil (CH)
Patient perspective
A. Pallaver, Nottwil (CH)
Across boundaries
S. Schibli, Nottwil (CH)
-
15:00 – 15:15
Petite pause sans repas
-
15:15 – 15:25
Gartensaal 1 A-C
Report Claude Verdan travelling fellowship
N. Zechmann-Müller, Winterthur (CH)My experience in Barcelona, Spain
C. Bouvet, Genève (CH)
-
15:25 – 16:30
Gartensaal 1 A-C
Special Session
Ohne Passion – keine Veränderung
E. Bodmer, Luzern (CH) / C. Struchen, Luzern (CH)Einführungsreferat: 4 Generationen – wie beeinflusst der Wertewandel die Handchirurgie und die Handtherapie
E. Bodmer, Luzern (CH) / C. Struchen, Luzern (CH)
Neue Generationen – veraltete Strukturen
F. Höpflinger, Horgen (CH)
Passion Gleichstellung als Motor der Veränderung
S. Banos, München (DE)
«No news, good news» war gestern: warum Generation Y eine neue Führungskommunikation braucht
S. Heuss, Olten (CH)
Diskussion
-
16:30 – 17:00
Pause café
-
17:00 – 18:30
Gartensaal 1 A-C
Réunion des membres SSCM
-
17:00 – 18:30
Gartensaal 2
Réunion des membres SSRM
-
19:30 – 22:00
Soirée de fête conjointe

