Herzlichen Dank an unsere Gold+, Gold- und Silbersponsoren:
Donnerstag, 28. November 2024
|
From 08:00
|
Registrierung |
|
|
Special
|
||
|
08:45 – 09:15
|
Gemeinsame Eröffnung |
|
|
Saal A
Sessions SGH/SGHR
|
Ivan Tami, Lugano; Ursula Osterwalder, Baden
|
|
Nimm mich bei der Hand – Prendimi per mano
Daniele Finzi Pasca, Lugano
In der Welt des Theaters ermöglichen uns kleinste Gesten, unserer Hülle abzulegen und in die Haut einer Figur zu schlüpfen. In der Akrobatik festigen dieselben Gesten unser Gleichgewicht und Vertrauen. Einander die Hand zu reichen, eröffnet eine Welt voller Möglichkeiten; auf der Bühne verwandeln wir dieses Verlangen in Anmut, Leichtigkeit und Poesie. Ein paar Worte zu meinem Handwerk, das ich stets mit Fingerspitzengefühl ausübe. Nel mondo del teatro minuti gesti permettono di svestirsi per entrare nei panni di un personaggio e questi stessi gesti nel mondo dell’acrobazia stabilizzano equilibrio e fiducia. Darsi una mano significa un mondo di cose, sulla scena noi trasformiamo questo anelito in grazia, leggerezza, poesia. Due parole sul mio mestiere che interpreto sempre in punta di mano. |
|
|
|
09:30 – 10:30
|
Freie Mitteilungen I |
|
|
Saal B
Sessions SGHR
|
Stefanie Kunz, Gelterkinden; Ingrid Cianci, Affoltern am Albis
|
|
|
FM60
Neue Wege in der Schmerztherapie – iPad-basierte Alternative zur Spiegeltherapie
Linda Meyer, Aarau
AbstractDie Handtherapie in Bellikon integriert die Spiegeltherapie in das multimodale Therapieschema für Personen mit chronischen Schmerzsyndromen oder Personen, die sich einer Amputation unterzogen. Dabei fiel mir bei der Evaluation auf, dass einige Klienten und Klientinnen die selbstständige Durchführung der Spiegeltherapie abbrachen. Auf Anfrage nannten sie folgende Faktoren: Probleme bei der exakten Platzierung des Spiegels entlang der Körpermittelachse sowie anhaltende rotierte Nacken – und Kopfposition für den Blick in den Spiegel. Folglich wurde von einer nachlassenden Fokussierung und der Unfähigkeit, die Illusion aufrechtzuerhalten, berichtet. Andere gaben an, ihnen fehle es an Motivation. Dies weckte das persönliche Bestreben, nach einer Alternative zur Spiegeltherapie zu suchen. Statt der konventionellen Spiegeltherapie, begann ich Videosequenzen von einfachen aktiven Bewegungen der nicht betroffenen Hand, mit dem iPad zu filmen. Diese Videos wurden mithilfe einer Bearbeitungsfunktion auf dem iPad gespiegelt, um die Illusion zu erzeugen, dass die betroffene Seite die Bewegungen ausführt. Es wurde eine kurze Testphase mit einem Klienten eingeleitet, der sich zunächst der konventionellen Spiegeltherapie unterzog und sich anschliessend alternativ die Videos ansah. Die positive Rückmeldung des Klienten sowie sein Interesse an einer ambulanten Weiterführung dieses Ansatzes, motivierte mich zur weiteren Erforschung dieser modifizierten Spiegeltherapie-Technik. Zielsetzung: Dieses Konzept zur möglichen Alternative der Spiegeltherapie mit dem iPad soll mit Literatur untermauert werden. Durch die Kombination von Erkenntnissen in der Praxis und der Literatur, können Richtlinien für das iPad-gestützte Trainingsprogramm formuliert werden. Diese Leitlinien sollen die Grundlage für die Einleitung einer Fallstudie, nach Beendigung der Projektarbeit, bilden. Methode: Als Grundlage diente eine Literaturrecherche, um Begründungen für den möglichen Effekt der Alternative der Spiegeltherapie zu finden sowie die Parameter des Therapieprogramms festlegen zu können. Die Recherche relevanter Literatur erfolgte in verschiedenen Datenbanken, darunter Medline/Pubmed, OTSeeker und der Cochrane Library. Ergebnisse: Aus den gewonnen Praxiserkenntnissen und der dazu gezogenen Literatur entstand ein Erhebungsfragebogen, ein Evaluationsbogen, ein Merkblatt und ein Therapieprotokoll für Klienten und Klientinnen sowie die Therapieempfehlung für Therapeuten und Therapeutinnen. |
|
|
|
FM61
Innovative Tools for Nerve Injury Rehabilitation: 3D-Printed Tactile Cube and Smart App Integration
Susanna Pagella, Lugano
AbstractHypothesis: In the context of nerve injuries, therapists employ Sensory Reeducation, a gradual and progressive reprogramming process of the brain utilizing cognitive learning techniques in the early phase and graded tactile stimuli in the subsequent phase. Patients often struggle to remember the materials and procedures, leading to inaccuracies in exercise execution, including incorrect timing, repetitions, and frequency. To address this, we designed a 3D-printed cube with various surfaces and developed an application “SensiReEduCube” to remind patients when to perform exercises and for how long. Methods: To encourage tactile stimulation in patients with nerve injuries, we designed a 3D-printed cube with each face featuring a different filigree. As therapists, we often lack information on whether patients have followed prescribed home exercises, particularly in cases where instructions vary based on pain levels. To ensure patient adherence and exercise accuracy, we created an application “SensiReEduCube” functioning as both a memo and an instructor. The application can be set as an alarm according to a therapist-determined schedule, with the therapist specifying the time the patient should spend on each face of the cube. The application guides the patient on when to rotate the cube, and a flag appears upon successful completion of each exercise. Results: Providing patients with a tool that motivates exercise coupled with an application offering precise exercise customization significantly enhances patient adherence to the treatment. The ability to monitor whether patients have completed exercises provides assurance regarding the effectiveness of our treatment instructions. Summary Points: By utilizing the cube, patients possess a visual reminder to perform exercises. The associated application allows for detailed customization of home exercises and provides feedback on execution, enhancing overall treatment efficacy. |
|
|
|
FM62
Implementierung von videobasierten Heimübungsprogramm-Apps in der Handtherapie
Eva Hege, Arbon; Michael Dieing, St. Gallen
AbstractHintergrund: Heimübungsprogramme (HÜP) sind ein wichtiger Bestandteil der Rehabilitation der oberen Extremität. Nur 35% der Patient*innen führen ihr HÜP konsequent durch. Angesichts dessen und durch zunehmenden Kostendruck der Versicherer ist es wichtig, ein attraktiveres HÜP zu gestalten, welches zu unserer modernen technologisierten Gesellschaft passt, um die Adhärenz der Patient*innen zu fördern. Ziel: Gegenüberstellung von videobasierten HÜP-Apps und einer konventionellen Abgabe eines papierbasierten HÜP, im Hinblick auf die Durchführungsadhärenz und die Qualität der Übungsausführung. Zusätzlich den Anforderungsbedarf an die Einführung von videobasierten HÜP in der Praxis zu eruieren. Methodik: Es wurde eine systematische Literaturrecherche durchgeführt. Zusätzlich wurden in unseren handtherapeutischen Abteilungen HÜP-Apps (Physiotec, Physitrack), am Beispiel der Nachbehandlung von Beugesehnenverletzungen eingeführt. Resultate: Basierend auf der durchgeführten Recherche bevorzugen die meisten Patient*innen ein videobasiertes HÜP. Dies führt zu einem verbesserten Verständnis der Übungen und einer korrekteren Durchführung. Eine ansprechendere Gestaltung der Übungen ist für eine zunehmend technologisierte Gesellschaft von Vorteil, um eine höhere Übungsadhärenz zu erreichen. Die vorliegenden Studienergebnisse geben einen vielversprechenden Ausblick. Es besteht jedoch weiterer Forschungsbedarf. Bei der Auswahl einer App ist es wichtig, den genauen Bedarf der Institution zu kennen und sich über die benötigten Funktionen zu informieren. Die Anpassung der Videos in den HÜP-Apps an die individuellen Nachbehandlungsprotokolle ist eine weitere Voraussetzung für eine erfolgsversprechende Nutzung in den Spitälern. Implikationen für die Praxis: Die Ergebnisse unterstützen die weitere Implementierung von videobasierten HÜP-Apps für individuelle Nachbehandlungsschemata in der Handtherapie, um die Therapietreue und die Ausführungsqualität der Übungen zu verbessern. Literaturverzeichnis: (weitere Literaturangaben in der Präsentation aufgeführt) Sheerin, M., Morrissey, A., Galvin, R., Ryan, D., Carey, L. & Robinson, K. (2023). Effectiveness of occupational therapy-led computer-aided interventions on function among adults with conditions of the hand, wrist, and forearm: A systematic literature review and meta-analysis. Hand Therapy (Online), 28(4), 133–143. https://doi.org/10.1177/17589983231209678 |
|
|
|
FM63
Brille der Zukunft - Virtual Reality in der Handrehabilitation
Sharon Viliotti, Münchenstein; Nina Keller, Zürich
AbstractHintergrund: Der stetige Wandel der Medizin und der Technologie ermöglichen bahnbrechende Innovationen. Virtual Reality (VR) bietet die Chance, die medizinische Versorgung zu revolutionieren. Durch das Eintauchen in die virtuelle Welt können die Patient:innenversorgung verbessert, medizinische Ausbildungen gefördert und Therapien optimiert werden. CUREO®, ein VR-Therapiesystem der Firma „CUREosity“, ist speziell für die kognitive und sensomotorische Rehabilitation entwickelt worden. Das Therapiesystem hat Potenzial für den Einsatz in der Handrehabilitation, das genauer untersucht werden soll. Ziel: Das Ziel des Projektes ist es, Stärken und Schwächen von CUREO® in der Handrehabilitation zu evaluieren und darauf aufbauend Entwicklungsvorschläge zu erarbeiten. Methodik: In einer zehnwöchigen Testphase mit 20 Patient:innen wurden die Stärken und Schwächen des VR-Therapiesystem mittels eines strukturierten Evaluationsbogens erfasst. Basierend darauf wurden Entwicklungsvorschläge erarbeitet, um CUREO® spezifisch für die Handrehabilitation zu erweitern. Diese wurden in einem Austausch mit dem Entwicklerteam von „CUREosity“ diskutiert. Resultate: Mit CUREO® können durch die realitätsgetreue Übertragung von Handbewegungen in die virtuelle Welt Alltagshandlungen simuliert und Handfunktionen spielerisch trainiert werden. Obwohl ein gesteigerter Handeinsatz bei den Patient:innen beobachtet werden kann, schöpfen die Spiele oft nicht das volle Rehabilitationspotenzial aus. |
|
|
|
FM64
ChatGPT and hand therapy: how AI can help in the treatment of epicoldylitis
Martina Ganzerli, Locarno
AbstractBACKGROUND Epicondylitis is one of the most common overuse syndromes, it affects people in working age and represents an economic and social burden. Symptoms can last for several months, recurrence is frequent (1, 2). The literature doesn’t offer well-defined protocols, but conservative treatment is considered the gold standard: adaptation of activities and physical therapy lead to significant improvements in pain, upper limb function and resolution of the problem in 90% of cases (1,3). ChatGPT, an artificial intelligence (AI)-based chatbot, can be used by the occupational therapist to create personalized rehabilitation programs for the patient using information such as age, job and functional limitations related to epicondylitis (4). OBJECTIVES The aim of this study is to evaluate the reliability of a rehabilitation program for epicondylitis proposed by ChatGPT compared to the conservative treatments found in literature. METHODS A literature review was conducted to reveal the best evidence for the treatment of epicondylitis. The results are compared with the ones produced by Chat GPT by inserting the string "give me an occupational therapy conservative treatment protocol for epicondylitis". RESULTS The treatment suggested by AI is comparable with evidence found in literature. ChatGPT can be used to give exercises specific for the patient's job. It’s always needed the supervision of a therapist capable of critically evaluating the results and the collaboration with the patient to share the further objectives and outcomes. More studies are required. BIBLIOGRAPHY 1. Stegink-Jansen, C. W., Bynum, J. G., Lambropoulos, A. L., Patterson, R. M., & Cowan, A. C. (2021). Lateral epicondylosis: a literature review to link pathology and tendon function to tissue-level treatment and ergonomic interventions. Journal of Hand Therapy, 34(2), 263-297. 2. Karabinov, V., & Georgiev, G. P. (2022). Lateral epicondylitis: New trends and challenges in treatment. World Journal of Orthopedics, 13(4), 354. 3. Kim, Y. J., Wood, S. M., Yoon, A. P., Howard, J. C., Yang, L. Y., & Chung, K. C. (2021). Efficacy of nonoperative treatments for lateral epicondylitis: a systematic review and meta-analysis. Plastic and Reconstructive Surgery, 147(1), 112-125. 4. Mittal, K., & Dhar, M. (2023). Use of ChatGPT by physicians to build rehabilitation plans for the elderly: A mini-review of case studies. Journal of the Indian Academy of Geriatrics, 19(2), 86-93. |
|
|
Diskussion |
||
|
09:30 – 10:30
|
Hauptsession IDefect coverage of the hand - Flaps vs. skin substitutes/skin grafts |
|
|
Saal A
Sessions SGH/SGHR
|
Florian Früh, Aarau; Martina Greminger, St.Gallen
|
|
Fingertip defect: Occlusive dressing
Urs Hug, Luzern
|
|
|
Fingertip defect: Local flap
Maurizio Calcagni, Zürich
|
|
|
Thumb defect, distal: Skin substitute/FTSG
Mathias Häfeli, Chur
|
|
|
Thumb defect, distal: Local flap
Pascal Ducommun, Cham
|
|
|
Hand, dorsum: Skin substitute
Alexandre Kämpfen, Basel
|
|
|
Hand, dorsum: Regional flap
Inga Besmens, Zürich
|
|
|
Cutting-edge microsurgical reconstruction of the hand
Bauback Safa, San Francisco US
|
|
|
|
09:30 – 10:30
|
Workshop A |
|
|
Saal C
Sessions SGHR
|
Sabrina Koch-Borner, Nottwil
|
|
Künstliche Intelligenz (KI) in der Handtherapie – praktische Anwendung verschiedener Tools für die Praxis
Bernadette Tobler-Ammann, Bern; Tamara Hauri, Bern
DetailsDie rasante Entwicklung der künstlichen Intelligenz (KI) hat das Potential, eine transformative Kraft in verschiedenen Bereichen der Medizin und Therapie zu sein. Das Ziel dabei ist es nicht, den Menschen zu ersetzen. Vielmehr soll sie unsere Fähigkeiten erweitern und uns im Arbeitsalltag unterstützen, um effizienter zu besseren Ergebnissen zu kommen. Insbesondere im Bereich der Handtherapie eröffnen sich mit der Anwendung von KI innovative Möglichkeiten, um die Effizienz und Wirksamkeit von Therapiemassnahmen zu verbessern und um uns in administrativen Aufgaben zu unterstützen. Ein praktischer Workshop zur Anwendung der KI in der Handtherapie bietet eine einzigartige Gelegenheit für Handtherapeut/-innen, sich mit den neusten Entwicklungen auf diesem Gebiet vertraut zu machen und ihre Fähigkeiten in der Anwendung von KI-gestützten Tools zu erweitern. Dieser Workshop richtet sich an Handtherapeut/-innen, die ihr Fachwissen und ihre praktischen Fertigkeiten im Umgang mit KI-basierten Technologien vertiefen möchten, um ihre Patienten noch effektiver zu unterstützen. Im Rahmen dieses Workshops werden die Teilnehmer-/innen die Gelegenheit haben, sich mit verschiedenen Aspekten der KI in der Handtherapie vertraut zu machen. Von der Nutzung von KI-Tools zur Bewertung von Handverletzungen, der erleichterten Suche nach aktuellen Studienresultaten für eine evidenzbasierte Praxis, der Entwicklung massgeschneiderter Therapieinterventionen bis hin zur Unterstützung im Formulieren neuer Flyers für die Praxis oder Heimprogrammen für die Patienten inklusive Übersetzung in Fremdsprachen bietet dieser Workshop einen umfassenden Einblick in die Möglichkeiten und Herausforderungen der Integration von KI im Praxisalltag. Praktische Fertigkeiten werden anhand von Fallbeispielen mit den drei kostenlosen KI-Tools «Humata», «ChatGPT» und «Evidence Hunt» trainiert. Daher müssen die Teilnehmer/-innen einen Laptop mit Internetzugang mitbringen und die Bereitschaft, ein kostenloses Login (Mailadresse; Passwort) für die drei OpenAI Tools für deren Nutzung zu erstellen. Darüber hinaus wird der Workshop Raum bieten für den Austausch von Erfahrungen und Best Practice im Umgang mit KI in der Handtherapie, um ein gemeinsames Verständnis für Chancen und Grenzen dieser Technologien zu entwickeln. |
|
|
|
10:30 – 11:00
|
Kaffeepause |
|
|
Pause
|
||
|
10:45 – 11:15
|
Narakas LectureNerves |
|
|
Saal A
Sessions SGH
|
Maurizio Calcagni, Zürich
|
|
Carpal tunnel syndrome and ulnar nerve entrapment - two ”compression neuropathies” with different biopsychosocial entities
Lars Dahlin, Lund SE
|
|
|
|
11:00 – 12:30
|
Freie Mitteilungen ICMC 1 |
|
|
Saal C
Sessions SGH
|
Nadja Zechmann-Müller, Winterthur; Cesare Fusetti, Bellinzona
|
|
|
FM1
Best and worst thumb CMC implant patients: Do they differ regarding their baseline characteristics?
Vanessa Reischenböck, Zürich
AbstractAim: The aim was to investigate whether patients with good outcomes after thumb carpometacarpal (CMC) joint arthroplasty differ in their baseline characteristics from patients with poor outcomes. Methods: Of 442 thumb CMC implant arthroplasties (Touch®, Keri Medical) documented in a prospective registry, 20 patients with the best and 20 patients with the worst 1-year outcome, measured by pain during daily activities, were selected. Baseline characteristics, i.e. age, sex, affected hand, Eaton stage of osteoarthritis, pain during daily activities (0-10, 0=best), brief Michigan Hand Outcomes (MHQ) questionnaire scores (0-100, 100=best) and key pinch strength of both groups were compared using the Mann-Whitney-U test. Median values with interquartile ranges (IQR) were calculated. Results: Patients in the best group had a 1-year pain score of 0 (IQR: 0) and patients in the worst group had a 1-year pain score of 7 (2). The baseline brief MHQ score was significantly higher in the best group (47 (21)) than in the worst group (36 (9), p≤0.01, figure 1). Similar results were found for key pinch strength where the best group had a baseline strength of 4kg (2) while the worst group had 3kg (2) (p≤0.01, figure 1). No differences were found between the groups in the other variables (p>0.05). Conclusion: Patients with better hand function before surgery have a higher chance to have less pain one year after thumb CMC implant arthroplasty. These findings underscore the importance of a thorough indication for surgery. It is important to consider that delaying surgery until symptoms worsen may result in poorer outcomes. 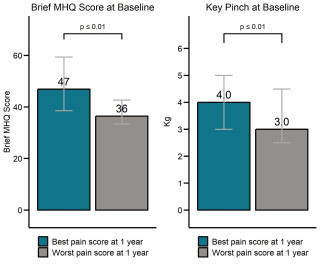
|
|
|
|
FM2
Automated analysis of TMC joint kinematics using four-dimensional computed tomography
Kjell van Royen, Aalst BE
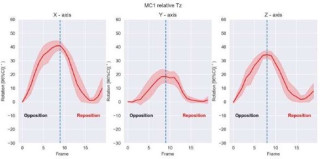
AbstractThe trapeziometacarpal (TMC) joint poses challenges in studying its kinematics due to its complex anatomy. Despite its susceptibility to osteoarthritis, our current understanding of TMC joint kinematics remains limited. Existing studies often utilize static computer tomography (CT) images, providing insights into the start and endpoints of specific movements but neglecting the dynamics during the movement. This study addresses these gaps by introducing a novel automated approach utilizing four-dimensional (4D) CT imaging to comprehensively analyze TMC joint kinematics during active opposition-retropulsion movements. The objective is to provide detailed characterization of TMC joint kinematics during an opposition-retropulsion cycle. Fifteen healthy volunteers with a mean age of 25 years, participated in the study. Volunteers underwent both static and dynamic scans, with the latter involving a cyclic opposition-retropulsion movement. Dynamic acquisitions consisted of 19 static scans per movement cycle. The image processing and motion estimation workflow incorporated automated segmentation and registration techniques. Motion of the thumb metacarpal relative to the trapezium, trapezium relative to the index metacarpal, and thumb metacarpal relative to the index metacarpal were described using cardan angles, representing flexion/extension, internal/external rotation, and abduction/adduction. TMC joint kinematics during opposition-retropulsion revealed detailed motion patterns for each bone involved. The position of the thumb metacarpal relative to the trapezium exhibited mean flexion of 41°, internal rotation of 21°, and abduction of 34° at terminal opposition. The trapezium's position relative to the index metacarpal showed mean flexion of 3°, internal rotation of 5°, and abduction of 5° at terminal opposition. Thumb metacarpal motion relative to the index metacarpal demonstrated mean flexion of 21°, internal rotation of 50°, and abduction of 19° at terminal opposition. In conclusion, this study introduces a novel and automated approach to analyze TMC joint kinematics during an active opposition-retropulsion movement using 4D CT images. The workflow significantly reduces processing time compared to previous manual analyses, addressing a major limitation in the field. The comprehensive analysis of TMC joint kinematics, hysteresis effects, and joint proximity dynamics provides valuable insights into the complex biomechanics of the joint. 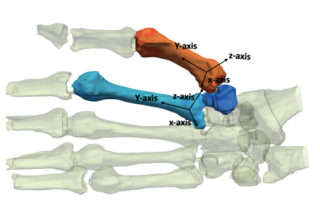
|
|
|
|
FM3
Analysis of trapeziometacarpal prosthesis cup position with respect to the trapezial anatomy.
Kjell van Royen, Aalst BE
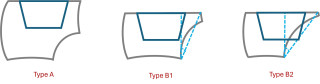
AbstractA trapeziometacarpal joint prosthesis is becoming increasingly popular in the treatment of symptomatic trapeziometacarpal joint osteoarthritis. The introduction of dual mobility designs has decreased the risk of dislocation, but incorrect cup placement is still a reason for concern. The purpose of this study is to analyze the anatomy of the trapezium with regard to cup position in trapeziometacarpal prosthesis and identify those trapeziums that are at risk for cup perforation in the trapezoid articular surface. The width of the proximal articular surface (PAST) and distal articular surface (DAST) and the height of the trapezium and second metacarpal facet were measured on 96 peritrapezial views. The TRAST angle was defined as the angle between the line connecting the most ulnar point of the PAST and DAST and the line perpendicular to the most ulnar point of the PAST. The TRAST angle was calculated for each trapezium and four different cup designs were virtually positioned central in the trapezium and parallel to the proximal articular surface of the trapezium. Risk of perforation was defined as a cup that exceeds the ulnar border of the proximal articular surface. Mean TRAST angle in our study was 33°. We introduce a classification to identify those trapeziums that are at risk for perforation. A type A trapezium has a second metacarpal facet height of more than 5 mm and has a low risk of perforation. A type B trapzium has a second metacarpal facet height of less than 5 mm. A type B1 has a TRAST angle of less than 35° and has a low risk of perforation. A type B2 has a TRAST angle of 35° or more and has a high risk of perforation. In our study, 19% is a type A, 50% is a type B1 and 31% is a type B2. When a type B2 trapezium is present, the cup could be positioned more radial or more distal to avoid perforation of the trapezoid articular surface. 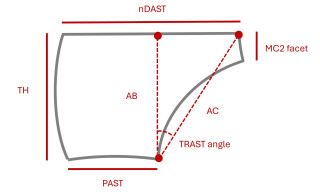
|
|
|
|
FM4
3D printed individual guide for centering the cup in TMC joint prosthesis - a proof of concept study.
Andrea Wenger, St.Gallen
AbstractIntroduction Since the invention of TMC-joint prosthesis some 15 years ago, several ball-in-socket prosthesis have been developed and clinical results are very promising. Still, most failures and revisions are due to loosening or dislocation. Duerinckx and Caekebeke (2016, 2017) described incorrect cup positioning as a contributing factor and postulated the intraoperatively central positioning of the cup essential for optimal results. Yet, guidelines for its orientation are not uniformly defined. During surgery, the positioning of the drill for the cup in the trapezium is the most critical part. The K-wire position is confirmed with intraoperative x-ray. To facilitate determining the centerpoint of the trapezium joint surface we tested the use of an individually 3D printed surgical guide to confirm the hypothesis that this will be more exact than positioning the cup without guide. Methods For the current proof of concept study preoperative CT scans were done on 20 cadaver hands as well as semi-automatic segmentation of the trapezium. The center point of the distal joint surface of the trapezium to the first metacarpal bone was calculated. A surgical guide for positioning the K-wire of the cannulated drill at the centerpoint of the trapezium was 3D-printed individually for 10 hands (Materialise, BE). Then, arthroplasty (MAIA prosthesis, Medkoh, CH) of the TMC-joint was done in the 20 cadaver hands using the individual guide in 10, the other 10 acting as control. Surgery was performed as in the routine clinical setting with intraoperative X-ray (Smart C, Swissray, CH). Postoperatively, another CT scan was obtained and the error to the centerpoint was calculated. Results For the guides group the postoperative centerpoint was obtained with an accuracy of 99,3% compared to the preoperatively calculated position and 98,3% for the control group respectively. The difference between groups was 0,64mm and 1,03% (not statistically significant). Discussion Although we could prove that positioning of the cup is more accurate with an individually 3D printed guide, our results were not statistically significant. This could be due to the small numbers of hands in each group. In the future we'd like to transfer the idea into daily surgery in patients with the objective to make TMC joint prosthesis safer and longer lasting in patients, since the cup positioning would be reproducibly optimal and therefore loosening or dislocation would be reduced to the minimum. 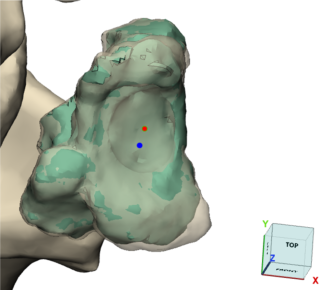
|
|
|
|
FM5
Thumb CMC total joint arthroplasty – Radiological comparison of spherical and conical cups at 1 year after surgery.
Bram van Hove, Leuven BE
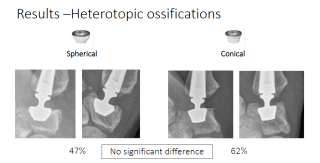
AbstractIntroduction Total joint replacement has become a reliable procedure for the treatment of trapeziometacarpal joint arthritis. Implant survival is reported to be between 15 and 25 years. Problems around the trapezial cup (loosening, fracture, ossifications) are the main indications for revision surgery. There is a variety of cup designs, but it is unclear which design is beneficial for long term survival. Objectives The goal of this study is to radiographically compare trapezial bone remodeling 1 year after implantation of a spherical or conical cup. We wish to objectively identify bony changes around the cup that might lead to implant failure. Methods We retrospectively evaluated radiographs of 106 patients at 1 year postoperatively of a trapeziometacarpal total joint replacement (Touch, Kerimedical, Geneva), operated between 2019 and 2021. Patients were selected to include that 53 had been implanted with a spherical cup and 53 with a conical cup. The decision to implant either implant is made peroperatively based on clinical findings. We evaluated the radiographies for bone resorption around the trapezial implant, subsidence, fracture, and heterotopic ossifications. Results We observed no cup tilt or dislocations, stage 1 loosening of 13% in spherical and 9% in conical cups, minor subsidence in 4% of spherical and in 4% of conical cups, observed the occurrence of heterotopic ossifications in 47% in spherical cups and 62% in conical cups. We found no difference between the two groups. Conclusion Our research showed that there is no clinical or radiological difference between the two types of cups. We observed a high occurrence of heterotopic ossifications in both groups. This warrants further long term follow up into the use of both cup designs. 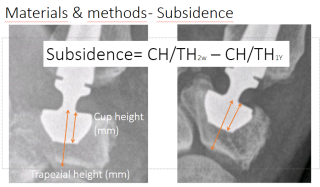
|
|
|
|
FM6
Does the cup shape matter for Touch® thumb CMC implants? Comparison of conical versus spherical cups
Vanessa Reischenböck, Zürich
AbstractBackground: The cup of the Touch® implant (Keri Medical) for the thumb carpometacarpal (CMC) joint is available in two shapes: A conical and a spherical cup. Aim: The aim was to investigate whether complications differed up to 1 year after implantation of the conical or spherical cup. Furthermore, we analysed 1-year clinical, radiological and patient-reported outcomes. Methods: Data from our registry, which prospectively documents all patients with a Touch® implant, were used. For the first 3 years, we only implanted spherical cups, as the conical was introduced later. Now, we routinely use the conical cup, as we believe it provides more intraoperative stability. For this analysis, each patient with a conical cup was matched based on their baseline characteristics with 3 patients with a spherical cup using propensity score matching. Data are shown as mean and standard deviations. Complication rates were compared using Fisher's Exact test. One-year outcomes of pain during daily activities (0-10, 0=best), brief Michigan Hand Outcomes (MHQ) questionnaire (0-100, 100=best) and key pinch strength between the 2 groups were compared using the Mann-Whitney U test. Results: Of 304 patients operated between May 2018 and March 2023, 72 had a conical and 232 a spherical cup. Revision surgery was done in 1 patient with a conical (1.4%) and 4 patients with a spherical cup (1.7 %, p=1.0). Intraoperative trapezium fracture did not occur during conical cup implantation but in 3 spherical cup implantations (1.3%, p=1.0). All fractures were successfully treated with a suture cerclage. 266 patients were available for the 1-year follow-up and 55 patients with a conical cup were matched to 165 patients with a spherical cup. Implant migration rates were 1.8% for both conical and spherical cups (p=1.0) and de Quervain’s tenosynovitis rates were 3.6% and 4.8% for patients with conical and spherical cups, respectively (p=1.0). There were no differences in the 1-year outcomes of pain during activities (2.0±2.6 vs. 1.6±2.0), brief MHQ (84±20 vs. 85±17) and key pinch (6.2kg±1.8 vs. 6.4kg±2.0) for the conical and spherical cups, respectively (all p>0.3). Conclusion: Complications, radiological and patient-reported outcomes at 1 year did not differ between patients with a conical or spherical cup. Therefore, we recommend use of either cup, depending on the surgeon's preference. |
|
|
|
FM7
Bone scintigraphic appearance of asymptomatic cementless thumb CMC total joint arthroplasty
Joris Duerinckx, Genk BE
AbstractImplantation of an uncemented total joint replacement requires osseo-integration for long-term stability. This process is dependent on increased bone metabolism with simultaneous bone absorption and new bone deposition around the implant. Depending on the transmitted load of the joint, this process may vary in time. Most studies describe normalization of bone metabolic activity on scintigraphy in asymptomatic cementless hip and shoulder joint arthroplasties between one and three years postoperatively. The normal evolution of bone scintigraphy after thumb CMC total joint arthroplasty is not known. To examine this, we performed a mono-centric study that included all patients who received a thumb CMC total joint arthroplasty between 2010 and 2022 and who had a bone scintigraphy postoperatively for another reason than pain in the operated hand. The time interval between surgery and scintigraphy and the amount of scintigraphic activity around the thumb implant were assessed for all patients. Knowing the normal evolution of bone scintigraphic appearance after thumb CMC total joint replacement is essential to allow correct interpretation of the results of this technical examination. |
|
|
|
FM8
The early complication rate of single versus dual mobility joint replacement of the thumb TMC joint
Pieter Reyniers, Antwerp BE
AbstractTrapezometacarpal (TMC) joint arthroplasty is becoming increasingly popular as a treatment option for thumb base osteoarthritis. Since its introduction by De la Caffinière in 1974, the design has evolved significantly, with a cementless, modular, ball-in-socket prosthesis now considered the gold standard. Good long-term survival rates have been reported with a single mobility, metal-on-polyethylene design, but the procedure is complicated by a relatively high complication rate, attributed to the learning curve and the high risk of dislocation. To address this issue, a newer dual-mobility design has been proposed, theoretically reducing the risk of dislocation. This study aimed to evaluate and compare the early (1-year) complication rates and outcomes of single-mobility (Arpe) versus dual-mobility (Touch) TMC joint prostheses. We conducted a retrospective review of patients who underwent TMC joint arthroplasty at our hospital between January 2018 and December 2022, including 336 procedures (168 Arpe and 168 Touch), all performed by a single surgeon. We recorded age, gender, occupation, and hand dominance. Patient satisfaction was investigated, as well as all complications that occurred in the first postoperative year. Preliminary data show that patient satisfaction is very high and similar in both groups. The most common complications in the Arpe group were instability with seven dislocations (4.2%), two trapezial fractures (1.2%), one cup loosening (0.6%), and one revision due to heterotopic ossification (0.6%). Five dislocations were reduced (one closed and four open); the other two required revision (head, and head and stem). All dislocations occurred within three months post-surgery. A much lower complication rate was found in the Touch group, with one dislocation (0.6%), successfully treated by closed reduction, one case of De Quervain tenosynovitis (0.6%), and one case of sensory radial nerve entrapment (0.6%). These results confirm the high early satisfaction rate of TMC joint replacement and the significantly decreased risk of early complications with the dual mobility design. Longer-term outcome studies will be necessary to confirm the long-term survival of these dual mobility design arthroplasties. |
|
|
|
FM9
Results of up to 2 years follow-up for Maïa™ dual mobility trapeziometacarpal joint prosthesis
Moritz Scholtes, Frauenfeld
AbstractIntroduction: Total joint replacement for trapeziometacarpal osteoarthritis (TMC-OA) is gaining popularity due to encouraging short and medium term results with high implant survival rates and excellent clinical outcomes. We report our short term outcomes and complications for the Maïa™ dual mobility TMC joint prosthesis. Materials/methods: All patients undergoing total joint replacement for TMC-OA from 02/2021 on were included in an ongoing patient register and examined preoperatively, at 6 and 12 weeks postoperatively and yearly thereafter. Parameters evaluated were patient demographics, TMC-OA stage (Eaton/Littler), thumb opposition (Kapandji score), grip and key pinch strength, pain score at activities of daily living ADL on visual analogue scale (VAS) and brief Michigan hand outcomes questionnaire (bMHQ). Complications and subsequent interventions including revision surgery were noted. Results: From 02/2021 until 04/2024, 34 patients were included, mean age was 62.7 years (range 40-81), 10 male and 24 female, 6 white collar, 14 blue collar and 14 retired. There were 9 patients with Eaton/Littler stage 2, 23 with stage 3 and 2 with stage 4. 34, 22, 23, 14, and 3 patients were available for preoperative examination, follow-up of 6 and 12 weeks and 1 and 2 years, respectively. Kapandji score was mean 8.9 (standard deviation SD 1.5) preoperatively, 9.3 (SD 1.0) at 12 weeks and 9.6 (SD 0.6) at 1 year. Grip strength was mean 22.2 (SD 10.7) preoperatively, 26.0 (SD 7.7) at 12 weeks and 26.8 (7.5) at 1 year. Key pinch strength was mean 5.2 (SD 2.6) preoperatively, 5.9 (SD 2.4) at 12 weeks and 6.3 (SD 1.5) at 1 year. Pain level at ADL was mean 8.2 (SD 1.5) preoperatively, 2.4 (SD 2.4) at 6 weeks and 0.8 (SD 1.9) at 1 year follow-up. BMHQ was mean 41.8 (SD 13.5) preoperatively, 84.1 (SD 22.0) at 12 weeks and 90.4 (SD 11.9) at 1 year. There was no dislocation or implant loosening. No prosthesis revision surgery was performed. Complications included one trigger thumb, one de Quervain’s tenosynovitis, one cup subsidence without loosening and one tendon adhesion, the latter three were treated surgically. Discussion: Treatment of TMC-OA with Maïa™ dual mobility TMC joint prosthesis shows excellent clinical short term results with low complication rates. Our data are comparable to the current literature on other dual mobility TMC joint prostheses. Short term outcomes for the Maïa™ dual mobility TMC joint prosthesis have not been published in Pubmed yet. |
|
|
|
FM10
What would you choose again - Thumb carpometacarpal implant or RSI arthroplasty?
Laima Bandzaite, Zürich
AbstractAim: The aim was to determine whether a thumb carpometacarpal (CMC) implant arthroplasty leads to higher patient satisfaction compared to RSI arthroplasty in the same patient. Methods: Patients who had undergone implant arthroplasty (Touch®, KeriMedical) in one thumb and RSI arthroplasty in the other thumb were invited to a follow-up visit. Patients completed a questionnaire including a satisfaction question, pain and the brief Michigan Hand Outcomes Questionnaire (MHQ). Key pinch and grip strength, range of motion and radiographic implant loosening were assessed at follow-up. Post-operative complications were extracted from medical records. Differences between the 2 hands were analysed using the Wilcoxon signed-rank test (continuous data) and Fisher's exact test (nominal data). Data were presented as median. Results: Fourteen women with bilateral surgery were examined at 2.2 and 6.2 years after implant and RSI arthroplasty, respectively. Ten patients would choose an implant again, 1 patient would choose RSI and 3 patients were undecided (p≤0.01). Twelve patients were satisfied or very satisfied with the outcome after implant arthroplasty, while 8 patients reported this level of satisfaction for RSI (p=0.41). Brief MHQ scores were higher in the hand with an implant arthroplasty compared to that with a RSI arthroplasty, as indicated by the respective scores of 81 and 71 (p=0.05). Key pinch (6.0kg) and grip strength (22kg) were significantly higher for the implant arthroplasty hands compared to the respective values of 4.5kg and 20kg for the RSI arthroplasty hands (p≤0.05). The other clinical and patient-reported outcomes did not differ significantly between the two hands at follow-up. Seven patients reported faster postoperative rehabilitation after implant arthroplasty than after RSI (p≤0.01). There were no complications or radiological loosening after implant arthroplasty, but two revision surgeries 1.5 years after RSI. Conclusion: Patients were satisfied with both procedures, but if they had to choose again, they would prefer implant arthroplasty. Implant arthroplasty provides at least similar medium-term outcomes to RSI, with faster rehabilitation, better hand function, greater strength and fewer complications after implant arthroplasty. |
|
|
|
FM11
Thumb CMC implant saves CHF 7'000 in lost productivity costs compared to RSI arthroplasty.
Kei Mathis, Zürich
AbstractBackground: Productivity loss measures the degree of work impairment due to health conditions, with its score ranging from 0% (no loss) to 100% (maximum loss). Aim: The aim was to investigate if patients treated with thumb carpometacarpal (CMC) implant arthroplasty have lower costs due to loss of productivity after surgery compared to patients with resection-suspension-interposition (RSI) arthroplasty. Methods: We used data from two prospective clinical trials and included employed patients who were treated with thumb CMC implant arthroplasty (Touch®, KeriMedical) or with RSI arthroplasty. Patients completed the Work Productivity and Activity Impairment Questionnaire to assess loss of productivity at baseline, and after 3, 6, and 12 months. Costs due to productivity loss were calculated by multiplying the productivity loss score by the monthly wage. Outcomes were compared between groups using an independent t-test and results are reported with mean and 95% CI (Confidence Interval). Results: 69 patients with implant arthroplasty and 46 patients with RSI arthroplasty were included. After implant arthroplasty, patients returned to work significantly faster, with a mean time of 51 days (43-59) compared to 84 days (50-117) for RSI arthroplasty patients (p<0.05). Productivity loss at baseline was 54% (48-60) and 47% (36-57) for implant and RSI patients, respectively and decreased to 10% (6-15) and 25% (15-35) one year after surgery (p<0.01, figure 1). The costs associated with lost productivity were significantly lower for implant arthroplasty patients over a one-year period, with CHF 15'781 (12'897-18'665) compared to CHF 22'707 (15'382-30'032) for RSI arthroplasty patients (p<0.05). Conclusion: Patients after thumb CMC implant arthroplasty returned faster to work and therefore, costs due to loss of productivity were significantly lower than after RSI arthroplasty. These findings are important in demonstrating that implant arthroplasty not only provides good treatment outcomes, but also has lower costs for the society. In negotiations with health insurers, these data can support the reimbursement of the cost of the implant. 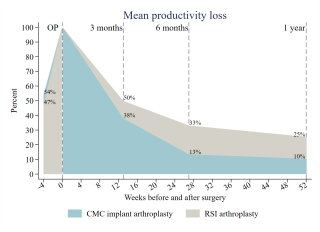
|
|
|
|
11:00 – 12:30
|
Freie Mitteilungen II |
|
|
Saal B
Sessions SGHR
|
Silvano G. Rech, Lugano; Livia Andrey, Biel
|
|
|
FM65
Relative Motion Orthosis bei Morbus Dupuytren - effektiv durch funktionellen Einsatz im Alltag
Manuela Schärer, Nottwil; Karin Szekeres, Bern
AbstractHintergrund Nach Fasziektomie, der häufigsten chirurgischen Behandlungsmethode bei Morbus Dupuytren (MD) in der Schweiz, beeinträchtigen oft postoperative Defizite im proximalen Interphalangealgelenk (PIP) die Handfunktion von Patient:innen. Die kostengünstige Relative Motion Orthosis (RMO) wird unter Handtherapeut:innen zunehmend als wirksame alltagsbezogene Übungsschiene zur Verbesserung von PIP-Gelenkbeweglichkeiten betrachtet. Obwohl die Schienenversorgung nach Fasziektomie kontrovers diskutiert wird und neue Studien die Vorteile spannungsfreier Mobilisation für Wundheilung und Handfunktion aufzeigen, bleibt das Potenzial des früh funktionellen Einsatzes der RMO dazu in der Handtherapie unerforscht.
Ziel Kann das konsequente Tragen einer alltagsbezogenen Übungs-RMO nach Fasziektomie zu einem möglichst frühen Zeitpunkt dazu beitragen PIP-Gelenkdefizite zu vermindern?
Methodik In der kleinen Fallserie mit Patient:innen nach Fasziektomie bei MD wurde ergänzend zu anderen Interventionen die RMO im Alltag eingesetzt. Zu festgelegten Messzeitpunkten wurden Beweglichkeit, URAM und PSFS, MCP-Differenzialwinkel mittels Pencil-Tests, ein Trageprotokoll sowie eine Tragekomfort-Auswertung erhoben.
Resultate Mit der RMO erreichten die Patient:innen 10 Wochen postoperativ eine Verbesserung der aktiven PIP-Beweglichkeit und Handfunktion. Aufgrund zusätzlicher Schienen ist die Zuordnung zur RMO nicht eindeutig. Der angenehme Tragekomfort und die einfache Alltagsintegration ermöglichen ein konstantes, nachhaltiges Beüben der PIP‘s.
Implikation für die Praxis Wir empfehlen, die RMO als ergänzende Intervention bei aktiven PIP-Gelenkdefiziten nach Fasziektomie, frühzeitig zu berücksichtigen. Zum Erreichen statistischer Signifikanz ist eine umfangreichere Fallserie mit Kontrollgruppe und Langzeit-Nachuntersuchungen erforderlich.
Literaturliste Turesson, C. (2018b). The Role of Hand Therapy in Dupuytren Disease. Hand Clinics, 34(3), 395–401. https://doi.org/10.1016/j.hcl.2018.03.008 Yates, S. E., Glinsky, J. V, Hirth, M. J., & Fuller, J. T. (2023). The use of exercise relative motion orthoses to improve proximal interphalangeal joint motion: A survey of Australian hand therapy practice. Journal of Hand Therapy, 36, 414–424. https://doi.org/10.1016/j.jht.2022.12.002 |
|
|
|
FM66
Welches ist das richtige Schienen-Design für Metacarpale-Frakturen?
Maria Fuchs, Thun
AbstractHintergrund Frakturen (Fx) der Metacarpalia (MCP) machen ca. 40% aller Knochenbrüche an der Hand aus (Häufigkeitsrate 13.6 pro 100‘000 Knochenbrüchen) (Keller 2024). Dabei kann der Knochen an der Basis, im Schaft, im Hals oder im Kopf brechen. Die Art der Fraktur (z.B. mehrfragmentär, Torsionsabweichung, Palmarverkippung, intraartikulär) hat einen grossen Einfluss auf die Wahl der Versorgung, wobei die Schienenanpassung eine zentrale Rolle in der Handtherapie spielt. Ziel Das Ziel dieser Präsentation ist es, den Behandlungspfad für MCP-Fx mit Fokus auf die Wahl der Schiene für MCP-Fx vorzustellen. Die verschiedenen Schienentypen werden diskutiert und vorgestellt. Methode Im März 2022 suchten wir nach aktueller Literatur zur therapeutischen Nachbehandlung von MCP-Fx. Diese wurde in einem aktualisierten Nachbehandlungsschema zusammengefasst und anschliessend mit den lokalen Zuweisern der Praxis besprochen, bis ein Konsens da war. Ergebnisse Das überarbeitete Nachbehandlungsschema dient als Nachschlagewerk, unter welchen Bedingungen welche Schiene angepasst werden soll. Für basisnahe MCP-Fx wird zum Beispiel eine vorderarmbasierte Handgelenkstütze aus thermoplastischem Material empfohlen, während die Schienenart bei den Schaft-Fx je nach Stabilität des Knochens variiert. Für Hals- und Kopf-Fx eignet sich eine handbasierte dorsale thermoplastische Schiene, welche das betroffene und benachbarte MCP-Gelenk sowie die Grundphalanx (P1) in 70° Flexion fixiert. Ein dazugehöriges Patienteninstruktionsblatt begleitet die Patienten während ihrer Genesung, so dass eine möglichst effiziente Nachbehandlung stattfinden kann. Implikation für die Praxis Ein klarer und aktueller Behandlungspfad für MCP-Fx hilft, evidenzbasierte Handtherapie anzubieten, die Kommunikation zwischen Arzt und Therapeut zu vereinfachen und somit den Patienten zielgerichteter nachzubehandeln. Nichtsdestotrotz sollte die Auswahl der Schiene auf einer klinischen Beurteilung beruhen und auf die spezifischen Bedürfnisse jedes Patienten abgestimmt werden. Literatur Keller MM, Barnes R, Brandt C, Hepworth LM: Hand rehabilitation programmes for second to fifth metacarpal fractures: A systematic literature review. S Afr J Physiother 2021, 77(1):1536. Midgley R, Toemen A: Evaluation of an evidence-based patient pathway for non-surgical and surgically managed metacarpal fractures. Hand therapy 2011, 16(1):19-25 |
|
|
|
FM67
Splint Selection in Carpal Tunnel Syndrome: Evaluating Lumbrical Involvement in Ticino, Switzerland
Susanna Pagella, Lugano
AbstractBackground: Carpal Tunnel Syndrome (CTS) is highly prevalent in Southern Switzerland's Ticino Region. Physicians commonly recommend conservative treatments before surgery, including nerve gliding exercises, ergonomic adjustments, and nighttime splinting. Diagnostic tests include Phalen's Test, Reverse Phalen's Test, and Durkan's pressure-provoking test. Incorporating the Berger Test may reveal lumbricals' role in CTS symptoms. Neglecting this assessment occasionally leads to inappropriate application of palmar braces. We aim to investigate this oversight's prevalence and gather regional data to enhance CTS understanding. Methods: We invited hand rehabilitation studies in Southern Switzerland to participate in our research on lumbrical involvement in CTS. Several studies contributed, adopting a specialized patient recruitment protocol. Non-surgically treated CTS patients underwent diagnostic tests, including the Berger Test. Test-positive patients received a targeted splint to prevent lumbrical accommodation within the carpal canal. We ensured standardized testing and data collection protocols across studies. A specialized patient recruitment assessment protocol was meticulously devised, focusing exclusively on distal median nerve entrapment. This protocol entailed the administration of diagnostic tests including the Phalen's Test, Reverse Phalen's Test, Durkan's pressure-provoking test, and the Berger test for all non-surgically treated patients diagnosed with CTS. Notably, patients who exhibited a positive response on the Berger Test underwent a targeted treatment approach. This involved the application of a splint designed to maintain the wrist in a slight extension at 20°, the metacarpophalangeal joints in flexion between 30° and 40°, and the interphalangeal joints at 0°. The purpose of this splint was to prevent lumbrical accommodation within the carpal canal. Uniform instructions were disseminated to all participating studies, ensuring a standardized and objective methodology for evaluating the Berger Test. Discussion: Our evaluation is ongoing but is revealing a clear distribution of positive cases across the region. Conclusion: If consistent, our survey will emphasize precise differential analysis of conservative CTS treatments, prompting tailored splint provision by hand therapists.
|
|
|
|
FM68
Fit für die Dokumentation von handtherapeutischen Behandlungen dank den FITT Prinzipien
Tamara Hauri, Bern
AbstractHintergrund Die Behandlung von Handverletzungen sind vielschichtig und umfassen verschiedenen Elemente: Patient:in, chirurgischer Eingriff und die postoperative Nachbehandlung. Sowohl in der frühen Phase als auch beim Aufbau der Belastung zielen diese Behandlungen darauf ab, das verletzte Gewebe gezielt zu beeinflussen für eine bessere Genesung. Dazu werden den Patienten spezifische Übungen instruiert, deren Intensität, Häufigkeit und Wiederholungszahl von Therapeut:innen festgelegt werden. Ziel Ziel des Vortrags ist es, mit den FITT Prinzipien ein Instrument vorzustellen, mit welchem sich die Nachbehandlung im klinischen Alltag und in der Forschung so dokumentieren lässt, dass die Reproduzierbarkeit gewährleistet wird. Methodik Die FITT Prinzipien werden erklärt und für die Handtherapie angepasst präsentiert. Anhand von Beispielen wird gezeigt, wie sie in der Praxis genutzt werden können. Resultate Die FITT Prinzipien werden im Trainingsbereich häufig angewendet. Für die Handtherapie könnte ihre Anwendung wie folgt aussehen:
Durch die Dokumentation des Übungsprogramms mit den FITT Prinzipien kann es von Kolleg:innen problemlos bei eigenen Patient:innen instruiert werden, von Studien in die Praxis übertragen oder in Studien reproduziert werden. Implikationen für die Praxis Die Anwendung der FITT Prinzipien bietet einerseits eine klare Struktur für die klinische Praxis, welche die Übertragung von Übungsprogrammen zwischen Patient:innen und Therapeut:innen ermöglicht. Andererseits erleichtert diese die Übertragung von Studieninterventionen in die Praxis. |
|
|
|
FM69
Spickfinger - macht Handtherapie Sinn?
Regula Harder, Wil; Heidi Senn, Bern
AbstractHintergrund: Die ergotherapeutische Behandlung von Tendovaginitis stenosans (Spickfinger) zeigt in der Praxis oft unbefriedigende Ergebnisse, da die Symptome bei einem Teil unserer Patient:innen erneut auftreten. Wir beobachten, dass auch eine Kortisongabe nicht immer dauerhaft wirkt. Daraus ergibt sich für uns die Fragestellung nach den effektivsten und nachhaltigsten handtherapeutischen Behandlungsmethoden für diese Erkrankung. Ziel: Analyse der aktuellen Evidenzlage und Ableiten handtherapeutischer Massnahmen. Methodik: Literaturrecherche in medizinischen Datenbanken und Fachbüchern. Resultate: Die vorhandenen Studien konzentrieren sich hauptsächlich auf Schienenbehandlungen und bekräftigen deren Wirksamkeit in Bezug auf verschiedene Schienenarten und Tragedauer. Andere Behandlungsformen wie physikalische Therapien, manuelle Mobilisation und Bewegungstherapie werden weniger häufig erwähnt. Unter Berücksichtigung der Pathophysiologie und klinischer Erfahrungen kann festgestellt werden, dass handtherapeutische Ansätze den Spickfinger positiv beeinflussen können. Praxisempfehlungen: Handtherapeutische Behandlungsmassnahmen sind gemäss Literatur in den unteren Einteilungsstadien der Erkrankung wirksam. Handtherapeutisch relevant sind die Schienenversorgung, ergonomische Beratung, physikalische Massnahmen, manuelle Gewebemobilisation und Sehnengleitübungen. Die Behandlungen sind an die individuellen Bedürfnisse der Patient:innen anzupassen. Abschliessend würden wir uns weiterführende Forschungen zu einzelnen handtherapeutischen Behandlungsansätzen zum Thema Spickfinger wünschen. |
|
|
|
FM70
Der springende Punkt beim Springfinger ist der richtige Zeitpunkt!
Maria Hodler, Thun; Chiara Naselli, Naters
AbstractHintergrund: Im ambulanten Setting werden erfahrungsgemäss Klient:innen entweder gar nicht oder zu spät zur konservativen Behandlung von Triggerfingern angemeldet. In der Literatur wird jedoch eine frühzeitige Anwendung einer massgefertigten Blockingschiene empfohlen. Mehrere Studien zeigen bei konsequenter Anwendung der Schiene, während eines durchschnittlichen Zeitraums von sechs Wochen, Linderung des Schmerzes und Reduktion des Triggerns auf. Ziel: Ziel dieses Projektes ist es, eine evidenzbasierte Informationsbroschüre zur Edukation von Klient:innen über die Effektivität einer frühzeitigen Schienenbehandlung des Triggerfingers zu erstellen. Methode: Zur Untermauerung des Projektes wurde eine Literaturrecherche in den Datenbanken Pubmed und Medline durchgeführt. Ein systematisches Review, eine randomisierte kontrollierte Studie, sowie eine Delphi-Studie liefern die evidenzbasierte Grundlage für die Broschüre. Resultate: Die Broschüre erklärt das Krankheitsbild in einer für Klient:innen verständlichen Sprache. Dazu gehört die Veranschaulichung der Stadien des Triggerfingers mittels einer Tabelle. Des Weiteren wird die Schienenbehandlung erklärt und bildlich dargestellt. Zusätzlich wird für Klient:innen die Definition der Handtherapie aufgeführt. Die Klient:innen können der Broschüre das Vorgehen für die Anmeldung zur Behandlung des Triggerfingers entnehmen. Anwendung für die Praxis: Die Broschüre ist auf den Institutions-Webseiten der Autorinnen frei zugänglich, kann heruntergeladen und ausgedruckt werden. Weiterführend wird die Broschüre an Hausärzt:innen der Einzugsregionen der Autorinnen zugestellt.
Huisstede, B. M. A., Hoogvliet, P., Coert, J. H., Fridén, J., & for the European HANDGUIDE Group. (2014). Multidisciplinary Consensus Guideline for Managing Trigger Finger: Results From the European HANDGUIDE Study. Physical Therapy, 94(10), 1421–1433. Leong, L., Chai, S. C., Howell, J. W., & Hirth, M. J. (2023). Orthotic intervention options to non-surgically manage adult and pediatric trigger finger: A systematic review. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 36(2), 302–315. Yendi, B., Atilgan, E., Namaldi, S., & Kuru, C. A. (2024). Treatment of trigger finger with metacarpophalangeal joint blocking orthosis vs relative motion extension orthosis: A randomized clinical trial. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, S0894-1130(23)00169-2. |
|
|
|
FM71
Mallet Finger Treatment and Results in 4 Different Treatment Scenarios
Anahi Jeanrenaud, Locarno
AbstractContext: Mallet finger deformities are caused by tendinous lesions caused by subcutaneous extensor tendon ruptures or bony lesions at the base of the distal phalanx with tendon avulsions. From our experience, conservative treatment stands as the gold standard. The aim of mallet finger treatment is to prevent long-term extension lag, flexion contracture of the distal joint, leading to swan neck deformity and joint osteoarthritis. We firmly believe that effective communication among surgeons, therapists, and patients is pivotal in achieving optimal functional outcomes. Together, surgeons and therapists must accurately assess various lesion types and define an appropriate rehabilitation protocol. The therapist is tasked with crafting the finger splint and administering the correct treatment while educating the patient. Objectives: Our objective is to illustrate different treatment scenarios that may have influenced outcomes following conservative treatment of mallet finger. Methodology: Four patients were diagnosed with acute tendinous mallet finger deformity. These patients were evaluated at two intervals: 8 and 12 weeks post-treatment initiation, with the splint removed after 8 weeks. Results: In one case, a non-compliant patient exhibited a 20° extension lag. In the second case, due to a shortened splinting duration (only 4 weeks), a 25° extension lag occurred. In the third case, a 20° extension lag resulted from an ineffective splint crafted by the hand therapist. Conversely, in the fourth case, successful outcomes were achieved, attributed to clear communication and compliance among surgeon, therapist, and patient. Conclusions: We present 4 scenarios delineating various treatment approaches for a common tendon lesion. Based on our experience, effective information exchange among surgeon, patient, and therapist is pivotal for optimal functional outcomes. This necessitates clear explanations from both the surgeon and therapist to the patient regarding the importance of adhering to the rehabilitation protocol, including guidance on the healing period. At times, the hand therapist must employ a customized rehabilitation approach to ensure the best possible outcome. |
|
|
|
FM72
Medical Flossing - Wirkungsnachweis anhand von Wärmebildaufnahmen
Bettina Bachmann, Herisau
AbstractHintergrund: Das Medical Flossing ist eine neuartige Therapietechnik, die in den letzten Jahren in den medizinischen Therapien Einzug gehalten hat. Im Bereich der degenerativen Erkrankungen zeigten sich kürzlich sehr vielversprechende Ergebnisse bei der konservativen Behandlung von Rhizarthrose (Plüss et al., 2024). Über die Wirkungsweise des Medical Flossings ist bekannt, dass es auf vier biomechanischen Prinzipien beruht: Myofasziale Kompression, Refill, Releasing und Movement Development (Kruse, 2018; Pischinger, 2021). Bislang ist es nicht gelungen, den Effekt des Medical Flossing nach ausschliesslich objektiven Kriterien zu beurteilen. Eine Möglichkeit ist die Visualisierung der Mikrozirkulation anhand der Temperatur im Gewebe direkt nach der Anwendung des Flossbandes. Fragestellung:
Methode: In einer Case Serie mit 5 Patienten wird die Technik des Medical Flossings im Rahmen der konservativen Behandlung bei Rhizarthrose standardisiert angewendet und die Veränderungen der Mikrozirkulation im Bereich des CMC-Gelenkes mit einer Wärmebildkamera festgehalten. Für weitere Vergleiche wurde die Patientenspezifische Funktionsskala (PSFS) und die Numeric Rating Scale (NRS) verwendet. Ergebnisse: Die Wirkung des Medical Flossings konnte anhand von Wärmbildaufnahmen visualisiert werden. Es kam bei jeder Anwendung zu einer Temperatursteigerung im Gewebe, wobei der grösste Anstieg jeweils nach dem ersten Durchgang erfolgte. Diese Ergebnisse lassen auf eine Mehrdurchblutung und somit auf einen erhöhten Zell- und Zwischenzellstoffwechsel schliessen. Bei vier Patienten wurde in der PSFS-Skala eine positive Veränderung und zugleich eine Schmerzreduktion festgestellt. Bei einer Person wurden die Beschwerden nicht gelindert. Implikationen: Das Medical Flossing beeinflusst den Stoffwechsel positiv und ist als Therapiemethode bei Rhizarthrose wirkungsvoll. Referenzen: Kruse, S. (2018). Easy Flossing. Thieme Verlag. Pischinger, A. (2021). Das System der Grundregulation. Thieme. Plüss, N., Bachmann, B. & Grünert, J. (2024). Medical Flossing bei Rhizarthrose - Verbessert eine mehrfache Wiederholung die Effektivität? DAHTH Zeitschrift für Handtherapie.
|
|
|
Diskussion |
||
|
11:15 – 12:30
|
Hauptsession IITraumatology of the forearm |
|
|
Saal A
Sessions SGH/SGHR
|
Mathias Häfeli, Chur; Christof Bollmann, Lausanne; Nadine Schulz, Zürich
|
|
Introduction
Mathias Häfeli, Chur; Christof Bollmann, Lausanne; Nadine Schulz, Zürich
|
|
|
Acute management of forearm fractures and injuries of the interosseus membrane
Christoph Sommer, Chur
|
|
|
Reconstruction of function in chronic foreram injuries
Andreas Schweizer, Zürich
|
|
|
Rehabilitation after forearm injuries
Mario Gaetano Fioretti, Lugano
|
|
|
Discussion |
||
|
12:30 – 13:45
|
Lunch and Networking |
|
|
Pause
|
||
|
12:45 – 13:30
|
Mittags-Symposium 1 |
|
|
Saal B
Symposium
|
||
CMC Prosthesis - 10 years of hindsight with the TOUCH by the designer
Cyril Falaise, St-Etienne FR
|
||
|
12:45 – 13:30
|
Mittags-Symposium 2 |
|
|
Saal C
Symposium
|
||
Radius Fixierung und Osteotomie
Andreas Schweizer, Zürich
|
|
|
Strategien bei komplexen Radius Frakturen
Frank J.P. Beeres, Luzern
|
||
|
12:45 – 13:30
|
Session Junge Handchirurgen SchweizSwiss Young Hand Surgeons |
|
|
Saal A
Sessions SGH
|
Mauro Maniglio, Zürich; Sophie Charlotte Brackertz, Basel
|
|
Welcome |
||
Jahresrückblick/ Bilan de l'année |
||
Diskussionsrunde/ Table ronde |
||
Klinik ledig sucht! - L'amour est dans l'hôpital
|
||
|
13:45 – 15:00
|
Freie Mitteilungen IIDistale Radius und DRUG |
|
|
Saal C
Sessions SGH
|
Lisa Reissner, Zürich; Daniele de Spirito, Lugano
|
|
|
FM12
Correlation Between Sigmoid Notch Morphology and TFCC Lesion in Distal Radioulnar Joint Instability
Flavien Mauler, Genève
AbstractIntroduction The stability of the distal radioulnar joint (DRUJ) depends, among other factors, on the morphology of the sigmoid notch. While variations in morphology have been relatively well described, specific data evaluating the correlation between the type of TFCC lesion and the morphology of the sigmoid notch are scarce. This study aims to describe the morphology of the sigmoid notch in patients treated for DRUJ instability and evaluate the correlation between joint morphology and TFCC lesion type. Methods Fifty-four patients treated for unstable DRUJ, who underwent preoperative arthro-MRI, were retrospectively included. The sigmoid notch was analyzed on T1-weighted MRI axial planes and categorized into four groups according to the classification of Tolat. This subjective classification was complemented with objective measurements and correlated with the shape of the radius and the curvature of the ulnar head. TFCC lesions were evaluated using preoperative arthro-MRI and arthroscopy. Spearman's correlation coefficients were used to assess the relationship between sigmoid notch morphology and TFCC lesion type. Results The morphology of the sigmoid notch in DRUJ instability was analyzed according to Tolat's classification. Objective measurements of the various morphology variations and their correlation with the type of TFCC lesion were assessed. Conclusion The shape of the sigmoid notch is a factor influencing the stability of the DRUJ. Correlation with the type of instability and TFCC lesion, as well as valuable insights for the surgical treatment of DRUJ instability are discussed. |
|
|
|
FM13
Ausmass einer Malunion des distalen Radius und Indikationsstellung für eine Korrekturosteotomie
Yves Waser, Zürich
AbstractEinleitung: In Fehlstellung verheilte, distale Radiusfrakturen sind oft mit einer Bewegungseinschränkungen oder einer Instabilität im DRUG einhergehend. Das DRUG ist an den Umwendbewegungen aber auch an der Kraftübertragung beteiligt, daher ist die Wiederherstellung der Gelenkskongruenz von Bedeutung. Dabei ist die Korrekturosteotomie die Therapie der Wahl. Mehrere Studien zeigten, dass mit 3D geplanten Korrekturosteotomien annähernd eine anatomische Rekonstruktion möglich ist. Bisher ist unbekannt, welches Ausmass an Korrektur (Achsabweichung und Translation) eine klinische Relevanz bzgl. Bewegungseinschränkung oder DRUG-Instabilität hat. Ziel dieser Arbeit ist, zu bestimmen, welches Ausmass an Fehlstellung notwendig ist, um postoperativ einen verbesserten postoperativen Outcome zu erreichen. Methodik: Alle Patienten zwischen 2017 und 2023, die an unserer Klinik eine Korrekturosteotomie bei einer fehlverheilter, distaler Radiusfraktur erhielten und ein Follow-up von mind. 6 Monaten hatten, wurden eingeschlossen. Die klinischen Daten wurden aus den prä- und postoperativen Routinekontrollen gewonnen. Der Fokus wurde auf die prä- und postoperative ROM, die klinisch getestete DRUG-Stabilität, die Faustschlusskraft sowie das Vorhandensein einer ulnaren Impaktionssymptomatik gelegt. Die Fehlstellungsanalysen und 3D Planung der Korrekturosteotomie wurden routinemässig erhoben und stammen aus der Spital-Plattform für medizinische Bildgebungen. Resultate: Insgesamt wurden 129 Patienten mit einem mittleren Alter 45 Jahren eingeschlossen, 82 Frauen und 47 Männer. Die mittlere Abweichung der Malunion in der Flexions-Extension-Achse betrug 14.67°(SD 10.95), radial/ulnar 7.04°(SD 5.34) und in Pro-/Supination 8.03°(SD 7.54). Eine durchschnittliche Verkürzung von 4.97mm(SD 2.67) wurde gemessen. Bei den bisher untersuchten 129 mittels Korrekturosteotomie operierten Fällen wurde bei 19 eine extraartikuläre Korrekturosteotomie mit einer Gradkorrektur von weniger als 10° in allen Ebenen durchgeführt und gute Ergebnisse bezüglich der ROM, klinisch geprüften Stabilität, der Faustschlusskraft oder der ulnaren Impaktionssymptomatik erreicht. Diskussion/Schlussfolgerung Unser Patientenkollektiv weist mehrheitlich Fehlstellungen mit einer dorsalen Abkippung von über 10° auf. Jeoch zeigt sich, dass bei entsprechender Symptomatik durch eine geringe Korrektur bereits eine substanzielle Beschwerdebesserung erreicht werden kann. Eine ausführliche Korrelationsanalyse wird am Kongress präsentiert. |
|
|
|
FM14
Stability of the distal radioulnar joint before and after corrective osteotomy of the distal radius
Lisa Reissner, Zürich
Abstract
Malunion of the distal radius with dorsal angulation increases instability of the distal radioulnar joint. The aim of the study was to sonographically quantify the instability of the distal radioulnar joint in 20 patients following corrective osteotomy of the distal radius and to investigate the subjective, clinical results preoperative, three and twelve months postoperative. Sonographically measured dorsovolar ulnar head translation relative to the distal radius was significant higher (3.6 mm) preoperative compared to 2.9 mm three months postoperative. Twelve months postoperative the result was 3.2 mm, similar to the contralateral side (3.3 mm). Pain, Disability of the Arm, Shoulder and Hand questionnaire and Patient-Reported Wrist Evaluations, wrist flexion, radial and ulnar inclination, grip strength and pronation and supination torque improved significantly. Corrective osteotomy of the distal radius shows good subjective and clinical results and a stable radioulnar joint sonographically measured. |
|
|
|
FM15
Dynamic Palmar Instability of the Distal Radioulnar Joint after Radius Shaft Malunion
Stefanie Schmitt, Luzern DE
AbstractIntroduction: Palmar instability of the distal radioulnar joint (DRUJ) is a rare condition, which is, in contrast to the dorsal dislocation, scarcely represented in the literature. This palmar instability can result from a dorsally angulated malunion of the radial shaft after forearm fracture in childhood. Treating such a condition is controversial in the literature and was described in small case series. This study represents the largest case series in the literature that dealt with this condition. Material and Methods: This is a retrospective case series. Ten patients were operated between 2007 and 2014. Six patients could be followed up clinically and radiologically after radius corrective osteotomy at the site of malunion with a mean time of 5.6 years. Patient history revealed a conservatively treated forearm fracture in childhood, a symptom-free period of several years [mean of 21.5 (min–max: 9.4–26.5) years] and a minor trauma as a trigger for clinical symptoms. All patients had clinically a DRUJ instability with palmar luxation of the ulnar head at supination. A diagnostic key feature was a radiograph of the whole forearm, revealing malunion of the radius at shaft level. Retrospective patient history, diagnostic imaging, operative technique and clinical results (DASH, modifed Mayo Wrist Score, pain, grip strength, range of motion) were analyzed. Results: Four patients were lost to follow-up. In all patients, a radius corrective osteotomy could stabilize the DRUJ. In all of the six patients, bony union of the osteotomy was achieved. In one patient, the osteosynthesis was revised due to metal failure after one month. In another patient, an additional ulnar shortening osteotomy was done one year later due to a positive ulnar variance. Postoperative range of motion of the wrist had an average of 136° in extension/fexion and 149° in pronation/ supination, and grip strength was 89% of the opposite side. With an average of 12.5 points at the DASH score and 82 at the modifed Mayo Wrist Score, patients rated their hand function as good. Conclusion: Dynamic palmar instability of the DRUJ is a rare and late complication after forearm fracture in childhood. A simple corrective osteotomy of the radial shaft was adequate to treat the complex pathology of a dynamic palmar instability of the DRUJ. A soft tissue procedure was not required. Medical history and a whole forearm radiograph were the key diagnostic features to detect and understand this rare pathology.
|
|
|
|
FM16
Improving Measurement Accuracy of Pronation/ Supination using Inertial Measurement Units
Michael Wirth, Zürich
AbstractIntroduction Pronation and Supination in the forearm occur during rotation of the radius over the fixed ulna in the proximal and distal radioulnar joint. The assessment of Pronation/ Supination range of motion (ROM) is difficult with a goniometer, so often it is simply estimated in clinical practice. Exact measurement is possible with an optoelectronic motion capture system (OMC) but due to its complex and time-consuming use, no clinical application is possible. Inertial measurement units (IMU) are accurate in flexion/ extension and radial/ ulnar deviation assessment and suitable for clinical use. We now tested a modified setup for Pronation/ Supination.
Methods Ten subjects with healthy right dominant hands were included and equipped with skin marker clusters for the OMC and with IMU sensors on hand and lateral epicondyle shown in Figure 1. IMU sensors were also equipped with OMC markers for direct comparison. Maximum ROM of five different trials and mean absolute difference between the two systems and between IMU and markers on the IMU sensors were calculated. The kinematic evaluation of the OMC was calculated according to an established protocol. The evaluation of the IMU was done by the manufacturer’s software.
Results The mean absolute difference of the ROM between the IMU and the OMC was 13 ° ± 8° and 7 ° ± 5 ° between IMU and OMC markers directly on the IMU sensors. The mean pronation/ supination ROM amounts to 145° when measured with the IMU, 157 ° with the OMC and 141° with OMC markers on the IMU sensors.
Discussion The observed differences between the IMU and the OMC show a systematic ROM underestimation by the IMU in the tested setup but high agreement between IMU and OMC markers on the IMU sensors, possibly due to skin movement over the lateral epicondyle during Pronation/ Supination. This hints to the need for an even more proximal sensor positioning. The study still shows the potential of IMU in measuring the complex Pronation/ Supination movement with high agreement between its results and the OMC markers directly on the sensors. 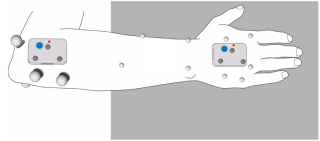
|
|
|
|
FM17
Minimalinvasive distale Radiusosteosynthese bei intraartikulären Radiusfrakturen (AO 23B1 – C3)
Dominik Spühler, Frauenfeld
AbstractEinführung Distale Radiusfrakturen gehören zu den häufigsten Frakturen und machen 12-17% aller Frakturen aus. Die Ergebnisse sind abhängig vom Schweregrad und Frakturmuster sowie der Therapiewahl. In den letzten 15 – 20 Jahren hat sich ein starker Trend hin zur operativen Versorgung mittels Plattenosteosynthese abgezeichnet, die eine frühfunktionelle Nachbehandlung mit sehr guten Ergebnissen ermöglicht hat. Die überwiegende Mehrheit der Frakturen kann mit einer winkelstabilen Platte von palmar versorgt werden. Jüngere Daten aus der Literatur deuten auf ein geringeres Komplikationsrisiko und ein besseres frühfunktionelles Outcome hin. Das Ziel dieser Studie ist es zu zeigen, dass der minimalinvasive Zugang auch bei komplexen Frakturen ausgezeichnete Ergebnisse liefert. Material&Methoden In die Studie haben wir Patienten/Innen eingeschlossen, welche von Januar bis April 2023 eine Osteosynthese am distalen Radius erhalten haben und folgende Einschlusskriterien erfüllen: minimalinvasiver palmarer Zugang von 1.5cm, distale fehlangulierte intraartikuläre Radiusfraktur und eine unterzeichnete Einverständniserklärung. Ausgeschlossen wurden Patienten mit Kombinationsverletzungen am ipsilateralen Handgelenk, extraartikuläre und konservativ therapierte distale Radiusfrakturen. Die primären Endpunkte waren der QuickDASH Score, die Kraftgrade im Seitenvergleich in Kilogramm (Jammar 2) und folgende radiologischen Parameter, welche anhand der konventionellen Röntgenbilder 6 Wochen und 3 Monate postoperativ gemessen wurden: palmare Inklination [°], Radiale Inklination [°], Ulnavarianz [mm] und Radiushöhe [mm]. Resultate Von Januar bis April 2023 wurden 52 distale intraartikuläre Radiusfrakturen (AO 23B1 – AO 23C3) operativ mittels palmarer Plattenosteosynthese minimalinvasiv über einen Flexor carpi radialis Zugang versorgt. Radiologisch zeigte sich eine anatomische Wiederherstellung des palmaren Tilts von 7° (0 - 15°), der radialen Inklination von 21° (10 - 32°) sowie der radialen Höhe von 10.5mm (7 – 13mm). Es zeigte sich eine neutrale Ulnavarianz. Der QuickDASH betrug 3 Monate postoperativ 21 und die Griffkraft erreichte 74% der gesunden Gegenseite. Konklusion Funktionell und radiologisch zeigen sich gleichwertige Resultate wie bei einem erweiterten modifizierten Zugang nach Henry. Die Osteosynthese der distalen Radiusfraktur über einen minimalinvasiven Zugang ist zuverlässig, komplikationsarm und zeigt kosmetisch ausgezeichnete Ergebnisse. |
|
|
|
FM18
WRIST – a stepwise intraoperative protocol to minimize complications in distal radial fracture osteosynthesis using a volar locking plate
Chul Ki Goorens, Tienen BE
AbstractAlthough outcome of volar plating is generally good, care should be taken to avoid specific iatrogenic and preventable complications, with an incidence reporting averaging 15%. Flexor tendon rupture due to a prominent plate, extensor tendon rupture due to a dorsal protruding screw tips, cartilage lesions due to intra-articular screw placement, loss of reduction due to insufficient stability, and persisting ulnar pain with distal radioulnar joint instability due to unstable triangular fibrocartilaginous complex lesions or unstable ulnar styloid base fractures all have been described. We believe that a majority of these complications can be prevented by meticulous assessment of several intraoperative parameters during volar plating. Therefore, we introduce the “WRIST” protocol, a stepwise manual that combines multiple fluoroscopic measurements to guide intraoperative decision making. The “WRIST” approach that comprises “wrist anatomy,” “range of motion,” “instability,” “Soong classification,” and “TFCC” is easy to remember. The “WRIST” checklist in OR theatre may avoid many complications of volar locking plating for distal radius fractures. In conclusion, large prospective studies of the "WRIST" protocol are needed for validation. But we believe that it may help surgeons to optimize surgical technique. functional and radiographic outcome, and prevent complications when treating distal radial fractures.
A Stepwise Intraoperative Protocol to Minimize Complications after Volar Plating. 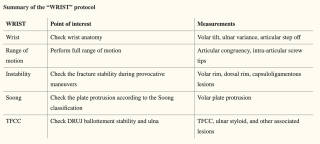
|
|
|
|
FM19
A series of 15 total wrist implants for acute distal radius fractures in elderly patients
Massimo Sammons, Gravesano
AbstractIntroduction: Despite advancements in surgical techniques and materials, we must acknowledge that we still encounter fractures that cannot be adequately addressed with a "standard" approach. Osteoporosis and diminished bone density can further complicate stable osteosynthesis. Here we present our experience with a series of 15 total wrist implants for acute complex distal radius fractures in elderly patients. Materials and Methods: Between September 2020 and March 2024, we treated 15 patients with complex DRF, comprising 3 males and 12 females, with an average age of 75 years (range: 63-83 years). Upon admission to the emergency room, patients underwent assessments, including radiographic (RX) and computed tomography (CT) scans. Utilizing the AO and Fernandez classifications, fractures were meticulously categorized, and associated lesions were identified. Following our algorithm for comprehensive fracture evaluation, we determined the most suitable treatment for each patient. Patients meeting study criteria underwent total wrist arthroplasty and received routine follow-ups at 6-week, 3-month, and 6-month intervals, during which X-rays were performed to monitor implant position, fracture healing, and osseointegration. Subsequently, patients completed the Disabilities of the Arm, Shoulder, and Hand (DASH) score and the Patient-Rated Wrist Evaluation (PRWE) test. The study spanned an average follow-up duration of 13 months, ranging from 6 to 31 months. Results: Our study reports satisfactory restoration of wrist mobility and grip strength (assessed using the Jamar dynamometer, averaging 16kg). At 6 months, the DASH score was 25.2, and PRWE was 15. Conclusions: In summary, it appears that this new implant can yield favorable functional outcomes. The prosthesis likely represents a viable option for managing complex distal radius fractures in a select patient population. However, confirmation of the indication for total wrist prosthesis requires a larger patient cohort and longer follow-up periods. While arthroplasty is one of the treatment options for wrist osteoarthritis, its role in wrist fracture management remains an evolving field. 
|
|
|
|
FM20
Outcomes of Radius Lengthening Osteotomy for Management of Premature Posttraumatic Radius Growth Arrest
Prisca Alt, Basel
AbstractBackground: Distal radius fractures are one of the most common injuries in children leading to posttraumatic radius growth arrest in 1-7%. Growth arrests can result in length discrepancy with ulnar overgrowth and functional impairment. Treatment options depend on length discrepancy, angular deformity and expected remaining growth. This study presents a case series of four teenage patients who underwent a radius lengthening osteotomy to manage posttraumatic radius growth arrest. We hypothesize that a good and painless range of motion and adequate length of the radius is achievable by radial lengthening if otherwise a length discrepancy of two or more centimeters between forearms is expected. Methods: We conducted a retrospective analysis of four teenage patients aged 14 ± 1.4 years with post-traumatic radius growth arrest secondary to distal radius fracture. All patients underwent radius lengthening osteotomy followed by external fixator distraction and subsequent plate fixation with iliac bone graft. One patient did not receive external distraction prior to plate fixation. Clinical and radiographic assessments were performed preoperatively, postoperatively, and at follow-up visits. Outcome measures included correction of radio-ulnar length discrepancy, improvement in range of motion, and assessment of complications. Results: Mean external distraction time was 8 ± 1.7 weeks, mean consolidation time was 13 ± 6 weeks until weight bearing commenced. All four patients demonstrated significant improvement in radio-ulnar length equality and range of motion following surgical intervention at the latest follow-up, which occurred at 20 ± 6 months. The mean radio-ulnar length discrepancy was reduced from 7 ± 5 mm preoperatively to -5 ± 3.5 mm postoperatively. Postoperative extension/flexion measured 75/0/70°, and pronation/supination measured 85/0/80°. Radiographic evaluation revealed successful correction of angular growth arrest deformity and restoration of radial length with no signs of ulno-carpal impaction. As complication we saw one delayed union leading to a reoperation without long-term impact on joint function. Conclusion: Radius lengthening osteotomy effectively restores radio-ulnar length discrepancy, and improves functional outcomes in wrist joint mechanics without lasting complications if a length discrepancy of more than 2 cm is expected. 
|
|
|
|
13:45 – 14:00
|
Report Forschungsfonds |
|
|
Saal A
Sessions SGH
|
Ivan Tami, Lugano
|
|
Sonography guided percutaneous release of the carpal tunnel
Saskia Kamphuis, Basel
|
|
|
|
14:00 – 15:00
|
Hauptsession IIISustainable hand surgery and hand rehabilitation! |
|
|
Saal A
Sessions SGH/SGHR
|
Mauro Maniglio, Zürich; Matteo Malacrida, Lugano
|
|
Why should a hand surgeon or hand therapist care about his footprint?
Anja Jost, Bern
|
|
|
Charting the Path: Advancements and Visions for an Eco-Friendly Swiss Healthcare System
Robin Sten Rieser, Bern
|
|
|
From Carbon Footprint to Carbon Handprint
Marie Jordan, Martigny; Matteo Malacrida, Lugano
|
|
|
Transforming My Hand Clinic into an ecological Oasis: Concrete Changes for Sustainable Hand Surgery
Leila Harhaus-Wähner, Berlin DE
|
|
|
The beneficial impact of Pre-operative Hand Therapy appointments for Trauma patients
Lucy Wimmer, Northampton GB; Emma Baker, Northampton GB; Dhanuja Senn, Northampton GB
|
|
|
Road to a carbon neutral Hand Surgery. Where are we in Belgium?
Mandala Senay Leliveld, Leuven BE
|
|
|
Tutti per uno, uno per tutti! Let's brainstorm together for a greener future
Matteo Malacrida, Lugano; Mauro Maniglio, Zürich
|
|
|
Diskussion |
||
|
14:00 – 15:00
|
Key Note LecturesMotor learning after Tendon and Nerve transfers: from theory to practice |
|
|
Saal B
Sessions SGHR
|
Silvia Schibli, Nottwil; Sabrina Koch-Borner, Nottwil
|
|
Basic Principles of Tendon and Nerve transfers
Armin Pallaver, Nottwil
|
|
|
Brain Plasticity
Karen Schmuck, Nottwil
|
|
|
The most common tendon and nerve transfers
Silvia Schibli, Nottwil
|
|
|
Steps of motor learning after tendon and nerve transfers
Sabrina Koch-Borner, Nottwil
|
|
|
Discussion |
||
|
15:15 – 16:30
|
Freie Mitteilungen III |
|
|
Saal B
Sessions SGHR
|
Tania Coli, Genève; Nicole Plüss, St.Gallen
|
|
|
FM73
Evidence-Based Treatment Methods in Focus: Successfully Navigating Scar Management in Hand Therapy
Tanya Schuhmacher, Zurich; Petra Hübscher, Schlieren
AbstractBackground: Scarring is a common consequence of skin injury or trauma, with significant implications for both physical and psychological well-being. Scar management aims to prevent abnormal healing processes, maximize functional independence, and facilitate patients' return to work while striving to restore them as closely as possible to their pre-injury state. Given the extensive literature on scar management, covering both non-invasive and invasive methods, and the integration of a wide range of these non-invasive methods into hand therapy practice, hand therapists are faced with a dilemma of determining the most suitable methods to use and optimal timing for their application. Therefore, careful assessment and selection of management methods are imperative. Factors such as scar type, patient-presented symptoms, wound healing phases, and patient background should all be taken into account. Aim: To provide a decision tree guiding informed decisions on various non-invasive scar management methods within hand therapy, specifically focusing on surgical and traumatic scars. Additionally, it seeks to evaluate the current evidence for each method to facilitate clinical decision-making for hand therapists. Methods: A literature review conducted through an electronic search across different databases such as PubMed, Cochrane, swissrecovery. Results and Implications: Scar management in hand therapy involves diverse methods with varying efficacy. Our review found inconclusive evidence for scar massage and dry needling, highlighting the need for standardized protocols. Meanwhile, challenges in treatment delivery persist for compression therapy, making its effectiveness difficult to establish. Cryotherapy and shockwave therapy show promise, and silicone dressings remain first-line options. Laser therapy, especially low-level laser therapy, significantly improves scar appearance and pain, while ultrasound therapy exhibits potential in tissue regeneration and inflammation reduction. Different types of tape effectively manage surgical scars, with high-stretch tapes potentially aiding wound healing. Cupping techniques enhance tissue improvement and may regulate hypertrophic scarring. Our review revealed that majority of studies focused on burn scars rather than surgical or traumatic scars. Further research is crucial for advancing scar management in hand therapy, informing therapists' clinical decisions, and refining tailored treatment approaches to provide more evidence-based interventions. |
|
|
|
FM74
Klinischer Fall mit Wundverschluss nach nekrotisierender Fasziitis: klinische Ansätze & Überlegungen
Ailsa Samin, Echandens
AbstractNekrotisierende Fasziitis (NF) ist eine schwerwiegende Infektion, die unbedingt einer chirurgischen Notfallbehandlung bedarf. Ein sekundärer Wundverschluss ist immer erforderlich und kann von der dünnen Hauttransplantation bis hin zum Verschluss mittels eines freien Hautlappens reichen. Bei jeder dieser Techniken fällt die Behandlung unterschiedlich aus. Solch heikle Situationen stellen die Handtherapeuten vor eine enorme Herausforderung: Hautlappen sind empfindlich und können nur begrenzt mobilisiert werden, während Transplantate aus dünner Haut nach medizinischer Freigabe bereits am fünften Tag mobilisiert werden sollten (1). Um die Herausforderungen zu veranschaulichen und Lösungen zu diskutieren, stellen der Chirurg und die Therapeuten hier einen klinischen Fall vor, der unser Vorgehen bei der Rehabilitation der oberen Extremität (OE) von der Hospitalisierung bis zum Erwerb der Selbstständigkeit beleuchtet. Wir präsentieren den Fall eines 47-jährigen Patienten mit NF an der OE, der einer Reihe von chirurgischen Eingriffen unterzogen wurde, u.a. unter Verwendung zweier freier Lappen sowie mehrerer dünner Hauttransplantate. Unser Behandlungsansatz umfasste verschiedene Methoden wie Narbenmassage, Lymphdrainage, Dermotonie, manuelle Therapie, Gelenkmobilisation, Orthesen und Silikone sowie Muskelaufbau. Objektive Auswertungen zeigten eine deutliche Verbesserung der Gelenkbeweglichkeit, Sensibilität und Muskelfunktion. Die Wundheilung war zufriedenstellend, mit einer erfolgreichen Integration der Dünnhauttransplantate. Nach mehr als einem Jahr intensiver Rehabilitation und zusätzlicher chirurgischer Verfahren erlangte der Patient vollständige Unabhängigkeit bei seinen täglichen Aktivitäten zurück. Diese Fallstudie unterstreicht die Bedeutung eines interdisziplinären Therapieansatzes bei Patienten mit chirurgisch behandelter NF. Intensive Rehabilitation in Verbindung mit einem effektiven Wund- und Schmerzmanagement sowie der engen Zusammenarbeit mit dem Patienten führen zu zufriedenstellenden funktionellen Ergebnissen und einer Verbesserung der Lebensqualität des Patienten. 1. Strohl AB, Levin LS. Management of Skin Grafts and Flaps: The Surgeon’s Perspective. In: Rehabilitation of the Hand and Upper Extremity. Philadelphia, PAE: Elsevier; 2020. p. 2112.
|
|
|
|
FM75
s’HAND-Gepäck – Ein Spielsachenset als Hilfsmittel zur Handuntersuchung bei Kindern
Myrthe Mali, St.Gallen
AbstractHintergrund: Manche Kinder wollen ihre Hände nicht untersuchen lassen. Mit dem gezielten Einsatz von Spielsachen ist es möglich gewisse Handfunktionen zu provozieren. In manchen Situationen fehlt es an geeigneten Spielsachen oder diese sind nicht schnell zur Hand. Fragestellung: Wie könnte eine Sammlung an Spielsachen gestaltet und zusammengesetzt sein, damit durch diese eine Handuntersuchung bei Kindern von 2 - 6 Jahren mit nicht akuten Handproblemen unterstützt werden kann? Methodik Verschiedene Spielsachen wurden basierend auf Erfahrungswerten und im Hinblick auf Aufforderungscharakter sowie Provokation bestimmter Handfunktionen mit Kindern mit und ohne Einschränkungen der Hände ausprobiert und ausgewählt. Der Bezug zur Theorie wurde mit Literatur untermauert. Ergebnisse: Entstanden ist das „HAND-Gepäck“. Ein kleiner Koffer mit ausgewählten Spielsachen, die mit Kindern zwischen 2 und 6 Jahren (Alter je nach Entwicklungsstand abweichend) in Handuntersuchungen genutzt werden können. Ergänzt wird das Set durch eine Anleitung und weitere Informationen. Implikationen für die Praxis: Das Spiel als eine der Hauptbetätigungen von Kindern und der gezielte Einsatz von Spielsachen können in der Handtherapie sowie Untersuchungssituationen unterstützend genutzt werden. Als positiver Nebeneffekt wird das gegenseitige Vertrauen gestärkt, was die Behandlung längerfristig erleichtern kann.
Hülsemann, W. (2019). Untersuchung der Kinderhand. Orthopädie & Rheuma, 22(3), 38–48. Laier, P., Haubold, J., & Weiss, E. (2011). Basisuntersuchung der Hand und Propädeutik. In Handchirurgie (pp. 13–25). Patane, G. R., Kanase, S. B., Bathia, K. J., & Patil, C. B. (2019). Effect of the Traditional Toys Exercises as an Adjunct to Hand Therapy Following Post-Traumatic Forearm Bone Fracture in Children. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, 13(4). Schelly, M., & Dunse, A.-L. (2023). Kindliche Handfehlbildungen in Ergotherapie und Physiotherapie. Van Nieuwenhoven, C., Laurell, T., Weber, D., Miller, C., & Guero, S. (2023). PULPe Webinar: Examining children’s hands. PULPe - Paediatric Upper Limb Project.
|
|
|
|
FM76
Beurteilungsbogen zur Dokumentation von postoperativen Narben (BDpN)
Zoé Franzen, Bruderholz ; Rebecca Amstad, Brugg
AbstractHintergrund Die Beurteilung von postoperativen Narben stellt einen bedeutenden Bereich in der handtherapeutischen Nachbehandlung dar. In unserem Arbeitsumfeld sowie der Literatur zeigt sich, dass hierfür häufig wenig standardisierte Assessments verwendet werden. Diese sind zudem hauptsächlich in Englisch verfasst und weisen unterschiedliche Entwicklungspotenziale auf. Es herrscht Uneinigkeit, welches Assessment sich am besten in der Praxis eignet. Basierend auf dieser Kontroverse entstand dieses Projekt zur Entwicklung eines neuen deutschsprachigen Beurteilungsbogens zur Dokumentation von postoperativen Narben. Fragestellung Wie gestaltet sich ein evidenzbasierter Beurteilungsbogen, welcher zur umfangreichen Dokumentation postoperativer Narben eingesetzt werden kann? Methode Die bestehenden Assessments zur Beurteilung von Narben werden einander gegenübergestellt und Entwicklungspotenziale erhoben. Ergänzend findet eine Literaturrecherche in diversen Datenbanken statt. Unter Einbezug der zusammengetragenen Aspekte wird ein neuer Beurteilungsbogen entwickelt. Die Erstversion dessen wird in der Praxis an zehn Klient*innen erprobt und anschliessend überarbeitet. Die verwendeten Bestandteile des Beurteilungsbogens werden zum besseren Verständnis in einem Leitfaden erläutert. Ergebnisse Es entsteht ein neu entwickelter Beurteilungsbogen zur Dokumentation von postoperativen Narben. Dieser vereint die Wahrnehmung der Fachpersonen der Handtherapie und der Klient*innen zu einem umfangreichen Bild. Der Beurteilungsbogen wird im Praxisalltag weiterhin erprobt und in digitaler Form bei der Befunderhebung und Verlaufsdokumentation von Narben eingesetzt. Schlussfolgerung Es stellte sich als Herausforderung dar, einen möglichst kurz gehaltenen Beurteilungsbogen zu erstellen, welcher alle wichtigen Aspekte beinhaltet. Die Umsetzung dessen zeigt, dass es möglich ist, die klinische Bewertung und die Sicht der Klient*innen zu vereinen.
|
|
|
|
FM77
Wunden in der Handtherapie: Welche Antiseptika eignen sich?
Marie-Ange Schneiders Spring, Lausanne
AbstractKontext. Handtherapeuten müssen häufig unterschiedliche Wunden behandeln. Zu entscheiden, ob eine Wunde vor der Wahl des geeignetsten Antiseptikums nur gereinigt oder desinfiziert werden sollte, ist integraler Bestandteil ihrer klinischen Überlegungen. Diese Entscheidung ist zentral bei der Behandlung eines solch empfindlichen Bereichs wie der Hand und spielt im Heilungsprozess eine bedeutende Rolle. Ziele. In diesem Vortrag soll die Bandbreite der auf dem Schweizer Markt verfügbaren Reinigungsmittel und Antiseptika vorgestellt werden. Ausserdem werden Empfehlungen zu bewährten Anwendungsmethoden in der Handtherapie abgegeben, um die verschiedenen Möglichkeiten aufzuzeigen, die eine optimale Behandlung von Patienten mit Wunden erlauben. Unsere Empfehlungen basieren auf einer vertieften Analyse des Konsensus von Kramer et al 2018, angepasst an die spezifischen Gegebenheiten und Bedürfnisse bei der Handtherapie. Praxisbezug. In Praxen und Krankenhäusern stehen Handtherapeuten in der Regel Reinigungslösungen wie NaCl mit oder ohne Antiseptikum in niedriger Konzentration sowie höher konzentrierte Antiseptika zur Verfügung. Wir haben sechs Hauptfamilien identifiziert: Chlorhexidindigluconat (CHD), Polyvinylpyrrolidon-Iod (PVP-Iod), Octenidindihydrochlorid (OCT), Polyhexanid (PHMB), Hypochlorite und Silberionen (Ag). Diese Präsentation soll einen praktischen Leitfaden für die gezielte und wirksame Wahl eines Antiseptikums bieten. Wenn Handtherapeuten die Besonderheiten der einzelnen Wundtypen möglichst gut kennen und deren Ursprung berücksichtigen, können sie das am besten geeignete Antiseptikum auswählen, um die klinischen Ergebnisse zu verbessern, das Infektionsrisiko zu senken und eine schnellere Heilung der Wunden ihrer Patienten zu fördern. Kramer, A., Dissmond, J., Kim, S., Willy, C., Mayer, D., Papke, R., . . . Assadian, O. (2018). Consensus on Wound Antisepsis. Skin Pharmaco Physiol, 31:28-58. |
|
|
|
FM78
Entwicklung, Etablierung und Evaluation einer Informationsbroschüre zur Prävention von CRPS
Verena Müller, Innsbruck AT
AbstractIn der Rolle der Gesundheitsfürsprecher:innen agieren Ergotherapeut:innen für Individuen, Personengruppen oder für die Bevölkerung mit dem Ziel, die Gesundheit zu erhalten bzw. zu verbessern (Peterko et. al, 2019). Unter der Projektleitung von Priv-Doz. Dr. Gernot Schmidle und Verena Müller wurde im Sommer 2022 gemeinsam mit sechs Ergotherapiestudentinnen des Bachelor-Studiengangs Ergotherapie (fh gesundheit Innsbruck) eine Broschüre zur Prävention von CRPS entwickelt. Im Rahmen des sogenannten berufsfeldorientierten Projekts der Studierenden wurde anhand der Literatur (Gillespie et al., 2016) eine Broschüre erstellt, bei der wichtige Hinweise nicht nur mündlich, sondern auch schriftlich an die Patient:innen weitergegeben werden:
Nach dem Corporate Design durch die Marketingabteilung sowie der Freigabe durch die kollegiale Führung der tirol kliniken wurde die Broschüre Mitte Februar 2023 eingeführt. Alle Patient:innen mit einem Gips an der OEX erhalten seither die Broschüre mit einem QR Code. Ziel der Broschüre ist es, die Patient:innen zu befähigen (empowern), die eigenen Beschwerden ernst zu nehmen und adäquat reagieren zu können, um so die Entstehung eines CRPS v.a. aufgrund von zu engen und einschneidenden Gipsen zu vermeiden. Die Broschüre ist Teil des interdisziplinären Behandlungspfades bei CRPS und dient der Prävention. Nach einem Jahr wurden die Zahlen erhoben und diese werden im Rahmen des Vortrages präsentiert, ebenso wie die weiteren Schritte (Plakate in Warteräumen, Übersetzung der Broschüre in weitere Sprachen wie Englisch und Türkisch, Beitrag Ambulanz TV, usw.).
Gillespie, S., Cowell, F., Cheung, G. & Brown, D. (2016). Can we reduce the incidence of complex regional pain syndrome type I in distal radius fractures? The Liverpool experience. Hand Therapy, 21(4), 123–130. Peterko, Y., Unterweger, K., Wagner, C., Stoffer-Marx, M., Dürauer, J., Lettner-Hauser, K., Manolopoulos, N., Nienhusmeier, B. & Garstenauer, C. (2019). Das Kompetenzprofil der Ergotherapie. Berufsverband Ergotherapie Austria. |
|
|
Diskussion |
||
|
15:15 – 16:30
|
Freie Mitteilungen IIIFinger Joints |
|
|
Saal C
Sessions SGH
|
Michaela Winkler, Lausanne; Alain Thebaud, Mendrisio
|
|
|
FM22
Treatment of skier's thumb without transection of the adductor aponeurosis
Yannick Goubau, Aalst BE
AbstractIntruduction: An injury to the ulnar collateral ligament (UCL) of the metacarpophalangeal (MCP) joint of thumb is a common injury, widely referred to as a skier’s thumb. The rupture usually occurs at the distal insertion. When the torn ligament displaces proximally, the aponeurosis of the adductor pollicis muscle can lie in the defect. Without anatomical reposition, the ligament cannot heal, and chronic instability will follow. In the classical technique, the adductor aponeurosis must be cut to repair the ligament to its insertion on the first phalanx, after which the aponeurosis is sutured back. Methods: We describe a technique to repair the UCL without transection of the adductor aponeurosis. We will provide professional artwork and video's. This technique might reduce articular stiffness and EPL tenodesis. We describe the use of this technique in 9 patients. Results: Mean active range of motion (ROM) in the MCP joint of the thumb was 52° of flexion and 4° of hyperextension. Resulting in a total arc of motion of 56 degrees, compared to 72° (59° flexion and 13° hyperextension) in the in the contralateral MCP joint. The median Kapanji score was 9/10 (range 8-10/10), in comparison, the median score at the non-operated thumb was 10/10 (range 9-10/10). Mean key pinch value came out at 6.67 kg (range 2-12 kg), on average of only 0.89 kg less than the contralateral side. Conclusions: Surgical repair of a UCL injury, with a Stener lesion, without transection of the adductor aponeurosis shows excellent clinical outcome both subjectively and objectively. When we compare our results to the literature, a tendency to better range of motion can be appreciated. Discussion: This technique is safe and relieable to repair a skier's thumb, and might reduce articular stiffness and EPL tenodesis. A prospective comparative study is needed to further investigate this. |
|
|
|
FM23
Aspects of therapeutic decision-making in bony skier's thumb injuries
Alina Strohmaier, Chur
AbstractIntroduction Acute tears of the ulnar collateral ligament (UCL) of the first metacarpophalangeal joint (MCPj) are common sports injuries. They are categorized into different types based on bony lesions, joint instability, and tear configuration (e.g. Stener lesion). Beside clinical examination, X-rays are standard to identify avulsion fractures. Dislocated fractures are often considered an indication for surgery. However, current literature lacks of criteria to classify a fragment as dislocated and the factors that influence the surgeon’s decision in these cases remain unclear. This observer trial aimed to identify aspects of therapeutic decision-making based on bony lesions in skier`s thumb injuries. Methods 75 X-rays of thumbs with bone fragments on the ulnar MCPj were evaluated by 6 observers (2 experienced and 2 resident hand surgeons, 2 radiologists). They determined whether the injury was osseous, dislocated, and recommended surgery or conservative treatment. The maximum fragment size, rotation, and the maximum/minimum distances to the proximal phalanx base were measured and correlated with the observer's decisions. The inter-observer reliability was assessed by Cohen's Kappa coefficient. Results Inter-observer agreement was substantial to identify bony lesions (0.71) and moderate for dislocation (0.51) and indication for surgery (0.49). Multilevel regression analysis showed that minimum distance and fracture fragment rotation significantly influenced the decision to classify a fracture as dislocated. Surgery was indicated more frequently with larger minimum distance or fragment rotation as well as when the lesion was categorized as dislocated. |
|
|
|
FM24
Improving patient information and decision making in management of stiff finger – a multimodal approach
Alissa Gübeli, Genève
AbstractIntroduction : After trauma or surgical procedures, many patients encounter digital stiffness, a common complication that severely disrupts both function and quality of life. The necessity of a surgical release of the finger and the postoperative outcome depends on numerous factors. We propose a multimodal approach with extensive pre-and postoperative assessment of the patients function and Patient Reported Outcome Measures (PROM) as a tool for decision-making, patient information and legal documentation, and present our clinical outcomes since 2022. Methods : In 2022, our institution implemented a protocol for assessing patients with stiff fingers due to trauma, infection, or surgery. It included evaluation of pain, range of motion (ROM), hand function and grip strength. Following surgery, patients received intensive physiotherapy, with frequency gradually decreasing over time, and re-assessments at 3 and 6 months post-surgery. We conducted a retrospective analysis on patients who underwent this protocol. Results : Between March 2022 and April 2024 above mentioned assessment was conducted on 27 patients who presented a stiff finger. Of these, 23 underwent surgical treatment. In four cases, conservative treatment was continued. Our analysis included 18 of the 23 patients who underwent surgery, with a follow-up assessment at minimum 3 months postoperatively. Their mean age was 43 years, 11 were female (61.1%), in 12 cases the dominant hand was affected. 12 patients unterwent tenoarthrolysis and 6 tenolysis. A palmar and dorsal approach was chosen for 12 patients, while 6 underwent a palmar approach only. In total, 24 fingers were operated, with 5 patients suffering from multidigital stiffness. The most commonly affected finger was the ring finger (33.3%), followed by middle (29.2%) and small finger (25%). At 6 months postoperative, there was a mean increase of total ROM of 39.7° per finger, a decrease of 11.9 points in the DASH score, an increase of 19.5% in the 400-point Hand Assessment, an increase of 10.3% in grip strength compared to the contralateral side and a decrease of 1.7 points in the Visual Analogue Scale. Conclusion : Thorough preoperative assessment of hand function including PROM in cases of stiff finger is invaluable for decision-making, patient education, and legal documentation. Our approach enhances collaboration with hand therapists, improves communication with patients, and ultimately aims to enhance clinical outcomes following tenoarthrolysis. |
|
|
|
FM25
Treatment of swan neck deformity after implantation of CapFlex prosthesis
Sarah Kerler, Goldach
AbstractSwan neck deformity is a rare complication after implantation of a CapFlex prosthesis. In the literature, its occurrence is known as a rare complication of the Chamay approach. We report on 4 patients who developed a swan neck deformity after implantation of a CapFlex prosthesis with a dorsal approach using the tendon splitting technique. As conservative treatment with splinting did not lead to improvement, surgical treatment was indicated. Different tenodesis techniques exist to correct swan neck deformity. We prefer a volar tenodesis using a FDS tendon slip as described by Bossé in 1981. According to his technique one slip of the flexor digitorum tendon is detached distally and passed through a drill hole in the proximal phalanx. After adjustment of the tension it is sutured to itself and the A2 pully. In contrast to the well-known tenodesis techniques described by Swanson or Tubiana, the Bossé tenodesis has a static and a dynamic effect at the same time: it serves as a pulley for the flexor digitorum profundus tendon and as a tenodesis for the proximal interphalangeal joint. Hyperextension in the PIP joint can thus be prevented without significantly impairing flexion. An early active rehabilitation program was started a few days postoperatively with dynamic splinting (Murphy ring). 6 weeks postoperatively all patients presented painfree and without functional restrictions. The PIP joint was stable in all cases. No recurrence of swan neck deformity occured so far. Swan neck deformity after implantation of a CapFlex prosthesis is rare and it can occur even years after the initial surgery. According to our experience, the tenodesis technique by Bossé is a simple and a biomechanically effective method when conservative treatment fails. |
|
|
|
FM26
Osteochondral autografts for PIP joint reconstruction in children with osteochondromas
Daniel Weber, Zurich
AbstractIntroduction Osteochondromas are common bone tumors in children’s hands. Complete resection is indicated due to angular deformity or restricted joint mobility. This destroys the articular congruity if the osteochondroma includes the articular surface. Primary reconstructions are controversial. The aim is to analyze a case series with primary joint reconstructions in children to report surgical outcomes and identify optimal autografts.
Methods This retrospective case series includes six children from two centers with a mean age of 7.2 (4 to 10.8) years with solitary osteochondromas of the phalangeal head of the proximal phalanx which were operated due to articular incongruity between 2015 and 2023.
Results All patients were reconstructed primarily with avascular osteochondral autografts, two from the base of the Vth metacarpal, two from the phalangeal head of proximal toe phalanx, and two from the hemimetatarsal head of the second toe. No recurrences were found during the follow up of 2.8 (0.3-8.5) years. All grafts integrated well with no signs of resorption. Patients did not complain about donor site defects or pain. All PIP joints were clinically stable and the active postoperative range of motion (ROM) [WD1] was 60 (25-90). All postoperative ROMs were equal or superior to the preoperative ROMs.
Conclusions Osteochondromas have a characteristic clinical and radiological presentation, allowing for primary reconstruction without prior biopsy in typical cases. Osteochondral autografts integrate well into the PIP with no bone resorption observed in the present series. All autografts resulted in stable PIP joints and the preoperative range of motion was restored or improved. However, the grafts from the base of the 5th metacarpal had the best congruity and did not need additional tailoring. Together with a minimal donor site defect and easy harvesting within the operative field, the 5th metacarpal base can therefore be recommended as a primary donor site. 
|
|
|
|
FM27
Finger kinematics and joint stiffness after treatment of intra-articular PIP joint fractures
Gabriella Fischer, Zurich
AbstractIntroduction: The aim of this study was to quantify PIP joint stiffness in patients after different treatment of intra-articular PIP fractures and to assess the relationship to finger kinematics.
Methods: Twenty-seven patients with intra-articular PIP joint fractures and a minimum follow-up time of 2 years were included and assigned to three different treatment groups: conservative, dynamic external fixation (DEF) or open surgical procedures (OSP, such as ORIF, arthroplasty, corrective osteotomy). Motion analysis was used to measure the range of motion (ROM) during dynamic finger flexion-extension. The stiffness of the affected PIP joint and the contralateral healthy side was measured using a newly developed finger stiffness measurement device. Axis deviation in the PIP joint was determined radiologically. PIP joint stiffness and ROM difference to the contralateral healthy side was compared between the different treatment groups (Kruskal-Wallis test, alpha=0.05). Pearson correlation was calculated.
Results: Median stiffness of the PIP joint was 0.0029Nm [0.0016-0.0066Nm] for the healthy and 0.0037Nm [0.0018-0.0057Nm], 0.0044Nm [0.0020-0.0055Nm] and 0.0049Nm [0.0028-0.0077Nm] in the DEF, conservative or OSP group, respectively. PIP joints were significantly stiffer after OSP, compared to healthy joints. Median ROM restriction of the PIP joint was significantly larger after DEF (82°) and OSP (79°), compared to conservative treatment (104°). In addition, a significant reduction of the DIP ROM (48°) and compensatory increase in movement of the MCP (113°) was observed after OSP, compared to the conservatively treated group (DIP 79°, MCP 103°). A significant correlation was found between increased PIP joint stiffness and PIP ROM (R=0.45, p=0.013) as well as DIP ROM (R=0.54, p=0.002), whereas MCP ROM correlated negatively with PIP joint stiffness (R=-0.44, p=0.016). Axis deviation tended to correlate with PIP joint stiffness (R=0.36, p=0.067).
Discussion: The ROM of the PIP joint was more restricted after surgical intervention (DEF and OSP) compared to the conservatively treated joints, while open surgical procedures additionally affected DIP ROM. Compensatory movements in the MCP >10° were observed in ~1/3 of the surgically treated fingers, but not after conservative treatment. However, different indications and a large inter-subject variability need to be considered. Overall, increased PIP joint stiffness correlates with restricted ROM in the PIP and DIP joint and with compensatory movement of the MCP. |
|
|
|
FM28
Reliable prediction of true metacarpal bone length - a novel approach
Sebastian Wangler, Bern
AbstractIntroduction Metacarpal (MC) fractures represent the most common fractures of the hand. Shortening can lead to active range of motion impairments of the metacarpophalangeal joints. The present study investigates the interobserver reliability of bone length measurements and presents a novel calculation method for predicting the correct length of metacarpal bones.
Methods A total of 60 X-rays of uninjured hands were identified. MC and phalangeal lengths of the index, long, ring, and little fingers were measured by three blinded observers using a clinical imaging system (Fig. 1a). Interobserver reliability of all measurements was calculated. Linear regression was used to identify the most significant correlation between the MC bone of interest and all other bones measured. The length of the strongest correlating bone was divided by the length of the MC of interest to identify a multiplication factor (x). As a proof of concept, the true length of all measured MC’s was compared to the calculated length by simple linear regression.
Results The mean age of the patient cohort was 54 ± 14 years, with 50% female. The interobserver reliability for all applied measurements was excellent (ICC 0.99, 95% CI: 0.99-1). The ulnarly neighboring MC was the most correlating bone for MC II-IV and the MC IV for MC V (p < 0.0001). Fig. 1b reports the multiplication factor x ± standard deviation (SD) for the identified correlations. A significant correlation between the measured and calculated MC V length was observed (p = <0.0001, R2 0.97) (Fig. 1c)
Conclusion The results of this study demonstrate excellent interrater reliability in the measurement of MC length in conventional X-rays. The ratios provided allow for a precise calculation of the true bone length, accurate to within 1.3 mm SD, based on adjacent MC’s. This approach may help to improve preoperative planning and intraoperative decision-making for surgeons treating metacarpal fractures or shortened fracture malunions. We plan to verify the concept and its clinical relevance in a prospective cohort study by standardized assessments of patients with MC fractures. 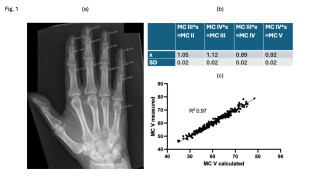
|
|
|
|
FM29
Determination of the Internal Loads in a Metacarpal Osteosynthesis during Rehabilitation Exercises
Tatjana Pastor, Davos
AbstractBackground: Metal plates used for metacarpal fracture fixation often lead to tendon adhesions and thus to an impairment in movement of the injured finger. To avoid tendon adhesion a new osteosynthesis material (AdhFix) has been developed. However, this new material has not been tested biomechanically in the metacarpal. Study aim: to investigate in a human cadaveric model the biomechanical potential of AdhFix used for fixation of metacarpal comminuted shaft fractures. Methods: The second, third, and fourth metacarpals in five cadaveric hands were instrumented using four stainless-steel cortical screws and a polyether ether kotone (PEEK) plate for treatment of an unstable metacarpal shaft fracture simulated by means of a 3mm osteotomy gap. A custom 3D printed cutting and drilling guide assured accurate screw placement and osteotomy cuts. The hand was stabilized in a supine position, and each digit's flexor digitorum profundus (FDP) tendon was extracted and connected to an electrodynamic testing apparatus (Acumen, MTS) via a steel cable. In order to replicate postoperative rehabilitation exercises after metacarpal fracture treatment, each tendon was pulled until the fingertip met the palm in its maximum flexion. Then, repeating the procedure with the flexor carpi radialis (FCR) and ulnaris (FCU) tendon, the wrist was flexed until a force of 100 N was reached. These tests were repeated 5 times each. The displacement of each PEEK plate was tracked with a stereographic camera system (Aramis SRX, GOM) throughout the tests. Finite element modeling (FEM) was employed to calculate the internal bending moment in the PEEK plate's midline during full finger or wrist flexion. Finally, AdhFix was applied after removal of the PEEK plate and the tests were repeated. Results: The maximum internal bending moments applied to the osteosynthesis during rehabilitation exercises were 6.14 ± 2.03 Nmm for fingertip to palm and 3.37 ± 1.64 Nmm for wrist flexion exercises as calculated by FEM. Additionally, the AdhFix fixations demonstrated resilience during these non-load bearing rehabilitation exercises on the metacarpal bone with no failures during the five of loading trials in the presented cadaver model. Conclusions: This biomechanical investigation combined with a subsequent finite element analysis, imparts a profound understanding of internal loads in metacarpal bones during non-weight bearing postoperative rehabilitation exercises, which AdhFix can withstand. 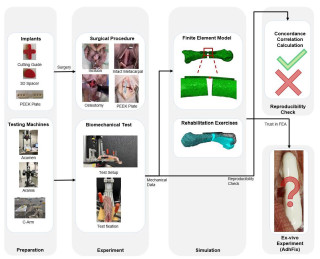
|
|
|
|
FM30
Ultrasound-based measure of dorsal scaphoid displacement during Watson test in SL ligament lesion
Nora Huber, Zürich
AbstractScapholunate ligament lesion (SLL) is the most common ligament lesion in the wrist. We assessed the reliability of sonography during Watson test (WT) in detecting SLL. 20 patients with MRI and intraoperatively confirmed SLL were assessed preoperatively between July 2020 and April 2023. Sonography was performed on the scaphoid dorsal subluxation (DS) in wrist neutral and during WT and compared with the healthy contralateral side. The DS was measured by two independent investigators and intra- and interobserver reliability were assessed. We found a statistically significant difference between DS of the scaphoid of the healthy (0.89 mm, SD 0.67 mm) compared to the pathological side (1.67 mm, SD 0.95 mm). Reliability was very good and SEM was lower than 0.4 mm for all measurements. Sonographic measurement during WT showed promising results with very good reliability; this method could be routinely adopted for the detection of SLL. 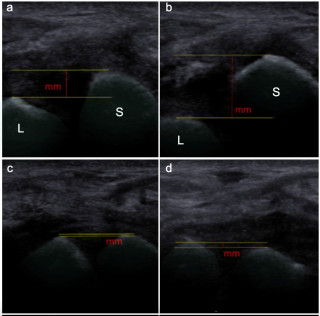
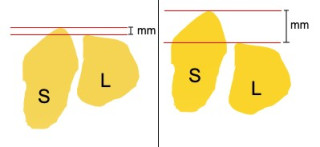
|
|
|
|
15:15 – 16:30
|
SGH Handfacts-Politpodium |
|
|
Saal A
Sessions SGH
|
Max Winiger, Zürich; Urs Hug, Luzern
|
|
Politpodium Expertenrunde
Walter Bosshard, Zofingen; Urs Hug, Luzern; Max Winiger, Zürich
|
|
|
|
17:00 – 18:30
|
Mitgliederversammlung SGH |
|
|
Saal A
Sessions SGH
|
||
|
17:00 – 18:30
|
Mitgliederversammlung SGHR |
|
|
Saal B
Sessions SGHR
|
||
|
From 19:30
|
Gemeinsamer Festabend |
|
|
Special
|








