-
08:00 – 18:30
Posteraustellung SGH
Measurement properties of the EQ-5D-5L questionnaire in patients after thumb CMC arthroplasty
M. Marks1, C. Grobet1, L. Audigé1 (1Zürich)
Show text
Background: The EQ-5D-5L includes only 5 questions and is the most popular questionnaire to assess quality of life. However, its measurement properties in hand surgery are not well investigated, yet, and it is unknown if it is sensitive enough to detect changes after thumb carpometacarpal (CMC I) arthroplasty.
Objective: The aim was to investigate the validity, responsiveness, minimal important difference (MID), minimal important change (MIC) and discriminative ability of the EQ-5D-5L utility index in patients after CMC I arthroplasty and to find out, whether the EQ-5D-5L would be a suitable instrument to measure quality of life in these patients, which is necessary e.g. for cost-utility analyses.
Methods: In this prospective study, patients with CMC I osteoarthritis completed the EQ-5D-5L questionnaire before surgery and 6 months and 1 year after resection arthroplasty. In addition, they filled out the brief Michigan Hand Outcomes Questionnaire (brief MHQ) and the Quick Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH). Construct validity (Pearson’s correlation coefficient, r), responsiveness (effect size), MID, MIC and floor and ceiling effects of the EQ-5D-5L were determined. To test discriminative ability, EQ-5D-5L utility indices of patients who were in a patient acceptable symptom state (PASS) or not at follow-up were compared using the Mann-Whitney U test.
Results: We included 151 patients with a mean age of 65 years (SD 8). The mean baseline EQ-5D-5L utility index increased from 0.69 (SD 0.19) to 0.87 (SD 0.15) at 6 months and 0.88 (SD 0.11) at 1 year (p≤0.001). The EQ-5D-5L utility index correlated well with the brief MHQ (r=0.61) and the QuickDASH (r=-0.64). Responsiveness of the EQ-5D-5L utility index was high with an effect size of 1.3. The MID was 0.027 and the MIC ranged from 0.090 to 0.209, depending on the calculation method. Seventeen percent of the patients achieved the highest possible score (1.0) at one year, indicating a light ceiling effect. The EQ-5D-5L utility index differed significantly between patients being in a PASS versus patients who were not in a PASS.
Conclusion: The EQ-5D-5L utility index shows good construct validity, responsiveness and discriminative ability in patients after CMC I arthroplasty. Despite the light ceiling effect, the EQ-5D-5L seems to be a suitable tool for quantifying quality of life in these patients, which is necessary to calculate quality-adjusted life years for cost-utility analyses.
The topography of the Anconeus nerve: a donor for transfer to the axillary nerve
M. Maniglio1, E. Zaidenberg2, E. Martinez2, C. R. Zaidenberg2 (1Lausanne; 2Buenos Aires AR)
Show text
Introduction
The anconeus nerve is the longest branch of the radius proximal to the sulcus, which facilitates its connection to the axillary nerve in Brachial plexus lesions. This makes him suitable as a donor side for the neurotization to the axillary nerve. The aim of this study was to take a precise look on the Anconeus nerve, his origin and insertions of the muscular branches and to map the topographical course of this important branch of the radial nerve.
Methods
We followed the radial nerve in 15 fresh frozen elbows specimens distally until the anconeus nerves was discernable. This point was defined as the apparent origin and was recorded. The anconeus nerve was further traced distally up to its entry to the anconeus. A concomitant innervation or nerve branches to the medial head of triceps brachii were visualized. The relation between the topographic course of nerve in reference to clear anatomical landmarks, all of which can be palpated precurtain with ease (Tip of the olecranon, medial and lateral epicondyle, intercondylar line (ICL)) were assessed.
Results
The Anconeus nerve separated with an initial diameter of average 1.5mm (SD: 0.2) from the radial nerve at about 16.4 cm (SD: 1.5cm) proximal to the lateral epicondyle, on the postero-medial side of the humerus. The nerve run between the lateral and the medial head of the triceps muscle, before entering the medial head ad an average of 10.2cm (SD: 2.4 cm) proximal the intercondylar line (ICL) and running intramuscular until to the distal humerus. Exiting the muscle for a short distance, the nerve lies on the periosteum of the distal humerus and the dorso-lateral articular capsule of the elbow joint, before entering the anconeus muscle with an average diameter of 0.5 mm (SD:0.1mm)
Two different types of Anconeus nerves were found: eight nerves innervate also the lateral head of the triceps and the other seven nerves only contribute two branches to his innervation.
Conclusion
Hand surgeons should, be aware of the course of the anconeus nerve, to know the option of this nerve as a valid donor side for the transfer to the axillary nerve. We want to underscore the critical passage of the nerve on the periost and the articular joint capsule, between the medial head of the triceps and the insertion into the anconeus nerve.
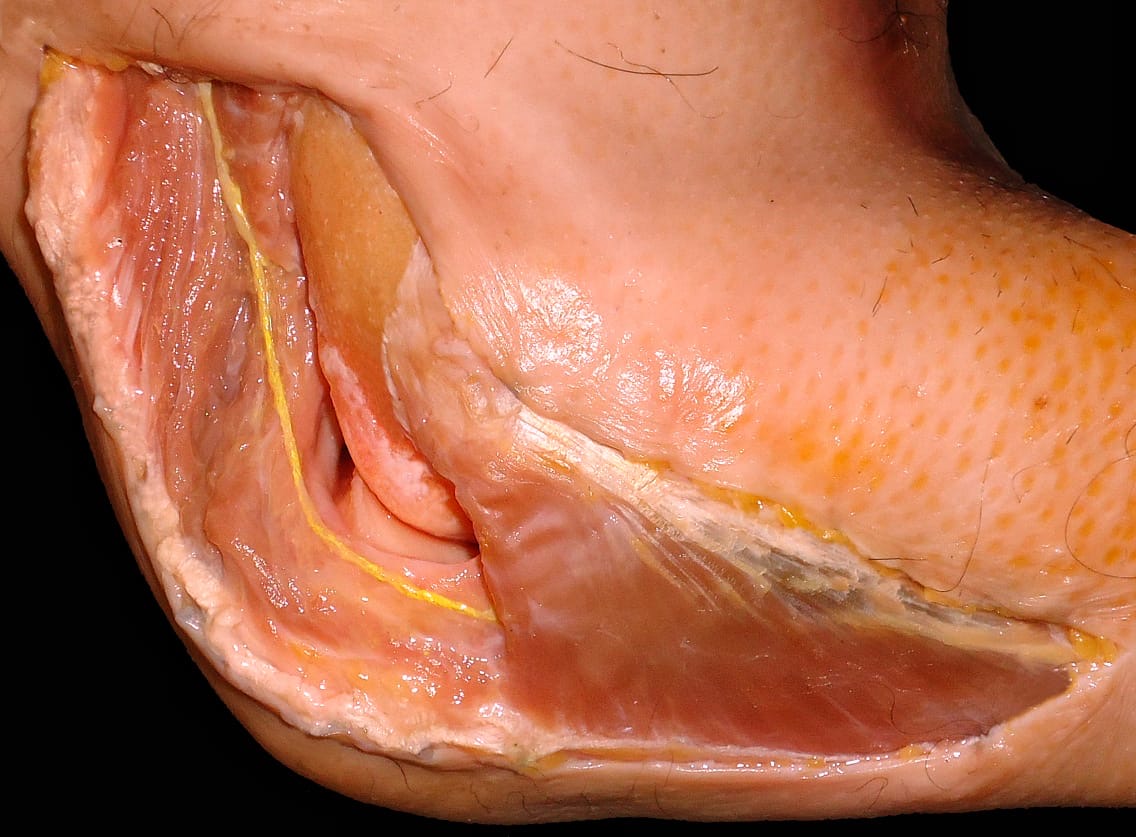
N. anconeus in the region of the elbow in yellow 
the Anconeus nerve in the region of the distal humerus 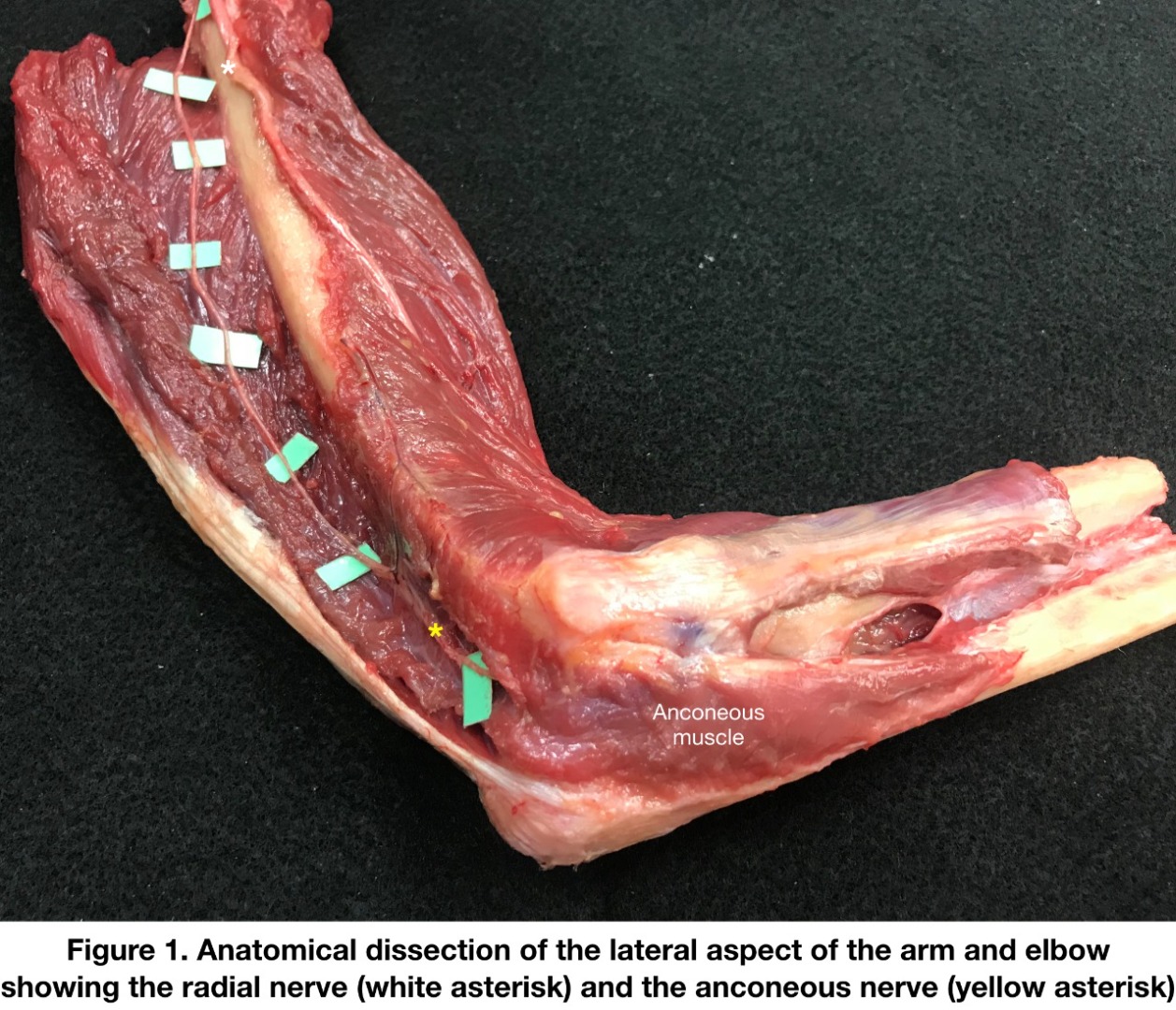
The course of the anconeus nerve in the humeral region Conservative Management versus Plating for Dorsally Displaced Distal Radius Fractures in the Elderly
M. Maniglio1, M. Tahir2, N. Ahmed3, A. R. Jamali3, G. Mehboob3, S. Khan4, A. Faraz5 (1Lausanne; 2Stanmore GB; 3Karachi PK; 4Prescott GB; 5Leeds GB)
Show text
Introduction:
Since the advent of the volar locking plate, the trend in the treatment of distal radius fractures (DRF) with dorsal displacement, in elderly patients, is towards the open reduction and internal fixation (ORIF) of unstable DRFs. However, the published literature is inconclusive and the choice of the best treatment is not certain. This randomized trial aims to compare the clinical, and radiological outcomes between plaster cast and volar plating for distal radius fractures in the elderly at 6 months, and 1-year.
Material and Methods:
A randomized trial was performed at a level 1 trauma centre between August 2016 and December 2019. The study included patients that were 60 years and above with an isolated, closed, unilateral, dorsally displaced DRF. Randomization into two groups (casting or plating) was based on a computer-generated algorithm stratified by age group and AO/OTA fracture type.
The primary outcome was Patient Rated Wrist Evaluation (PRWE) score. Secondary clinical outcomes were active range of motion, grip strength, the Mayo’s wrist score and the quick Disability Arm, Shoulder, Hands scale. Patient’s satisfaction was evaluated with use of a SF-12 questionnaire and finally complications were recorded.
Results:
This pragmatic randomised controlled trial has shown that there is no significant difference in clinical outcomes of DRF at 6 and 12 months follow up when treated by cast immobilisation or plating. Although, the radiological parameters and the number of complications were significantly higher in the immobilisation group.
Conclusion:
To conclude, the results of the trial have shown that plating and casting are equally effective in achieving satisfactory patient reported and clinical outcomes at intermediate and final follow-up. Restoring patient satisfaction.
Intraoperative stability of the first carpometacarpal joint
P. Behm1, M. Marks1, S. Ferguson1, M. Brodbeck1, D. B. Herren1 (1Zürich)
Show text
Objective: There are no quantitative data on the intraoperative stability of the thumb carpometacarpal (CMC I) joint after trapeziectomy and the amount of added stability after tendon suspension and interposition (resection-suspension-interposition arthroplasty [RSI]). Therefore, our study objective was to measure CMC I joint stability during RSI. The contribution of the various surgical steps to stability was analysed and its relation to preoperative clinical and patient-reported measures was assessed.
Methods: Preoperative pinch grip, thumb mobility (based on the Kapandji score) and hypermobility (using the Beighton score) were determined. In addition, patients completed the brief Michigan Hand Outcomes Questionnaire. During surgery and upon removal of the trapezium, the surgeon subjectively rated the degree of CMC I stability either as “stable”, “medium stable” or “unstable”. A measurement system with integrated force sensor was used to measure intraoperative CMC I stability. Briefly, a reposition forceps was attached to the base of the MC I and to a linear slide with integrated force sensor in a standardized pinch grip position. The thumb ray was displaced manually by 10 mm towards the scaphoid and the counteracting force measured over the entire displacement. Objective stability was determined as the maximal measured force after trapezium resection, tendon suspension and interposition.
Results: We included 29 patients with a mean age of 70 years (±8.1). From the subjective surgeon ratings of stability, there were 13 (45%) thumbs considered as stable, seven as “medium stable”, and nine were considered unstable after trapeziectomy alone. These subjective ratings did not correlate with the objective stability measurement (r=0.28). In addition, none of the evaluated clinical or patient-reported variables correlated highly with the objective measurement. The objective intraoperative stability after trapeziectomy was 15.5 N (SD 5.4) and significantly increased to 18.7 N (SD 5.5) after suspension (p≤0.001). Stability only slightly increased after tendon interposition with an increase in force to 20.3 N (SD 6.7; p=0.124).
Conclusions: The results of our study show that suspension contributes the most to thumb stability during RSI arthroplasty. Tendon interposition does not seem to have a significant additional effect regarding stability, at least immediately after surgery.
Long-term follow-up after first dorsal extension osteotomy in early thumb carpometacarpal arthritis
E. Coppo1, P. Honigmann1, D. Sutter1 (1Liestal)
Show text
Preliminary results
Purpose: To evaluate the long-term outcomes and survival of first metacarpal extension osteotomy (Wilson osteotomy) for early thumb carpometacarpal (CMC) arthritis.
Methods: Patients who underwent an extension osteotomy of the first metacarpal in our department between years 2013 and 2020 were identified. Demographics, complications, and reoperations were recorded. These patients will be enrolled for a follow-up examination in the outpatient clinic. The Patient Rated Wrist/Hand Evaluation (PRWHE) and the Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaires will be submitted to each patient. Further clinical evaluation will include the following criteria: pain, palmar abduction of the thumb, carpometacarpal joint opposition of the thumb (Kapandji), range of motion of the metacarpophalangeal joint and strength. Progression of osteoarthritis will be evaluated on follow-up radiographs.
Results: On retrospective analysis, 46 procedures in 39 patients (7 males and 32 females) were identified (mean age, 45.7 y, mean follow-up 11.6 months, range 3-36 months, 79.5% dominant hand). Analysis of patient records showed no cases of nonunion. 22 of 46 thumbs underwent removal of the osteosynthesis material (47.8%). In 36 out of 46 thumbs were reported little to no pain at last follow-up (78.2%). 10 patients reported persistence or progression of their symptoms. In 7 thumbs was observed a radiological progression of arthritis according to the Eaton-Littler classification (15.2%). All these patients were symptomatic and underwent or were recommended to a revision (overall 15.2% revision rate, either trapeziectomy or arthroplasty). 40 thumbs (87.0%) retained a Kapandji score for carpometacarpal joint opposition of 8 or more, full extension in CMC I was always achieved.
Conclusions: Retrospective data suggests good pain relief with high patient satisfaction in short-to-mid term follow-up after first metacarpal extension osteotomy. A 15.2% progression rate of arthritis was observed, corresponding with the revision rate. These rates give reason to hope for good long-term results in first metacarpal extension osteotomy for early thumb carpometacarpal arthritis.
Treatment of fracture dislocation of the proximal interphalangeal joint with a new external fixator
C. Bouvet1, J. Y. Beaulieu2, K. Liu3, J. van Aaken2 (1Sierre; 2Genève; 3Beijing CN)
Show text
Background: Fracture dislocation of the proximal interphalangeal joint is a challenging situation, to face this situation the hand surgeon must be aware of all the surgical technic to deal with the joint instability. Management of the palmar comminution is a key process in the joint stability. Dynamic external fixator allows rapid motion to avoid joint stiffness. We describe the surgical technique and the clinical results of a new device: the Gexfinger®. It is an elastic dynamic external fixator which not only allows for motion of the PIP joint but also preserves elasticity of the ligaments and capsule during the distraction period
Methods: This is a retrospective study, between 2017 to 2019 in 3 centers. We collected the clinical data from 26 patients who benefit from the Gexfinger®.The study was conducted in 3 centers in 2 countries.
Results: For 26 patients, mean arc of motion of the PIP joint was 82° (60°-110°), for the DIP joint 65° (55°-80°). Grip strength in comparison with the contralateral side was 83%. All patients got back to work at a mean time of 7 weeks (2 to 12 weeks). We had 2 patients with PIP joint stiffness. Seven patients had only the external fixator, 15 patients benefited from additional screw 3 needed additional Kirschner wire and 1 patient benefit from screw and Kwire. The external fixator was left in place during 5,5 weeks. The mean follow-up was 8 months. Fifty-six percent of patients were very satisfied, 32% satisfied and 12% unsatisfied.
Conclusions: For fracture dislocation of the PIP joint we advocate the use of a dynamic external fixator in association with ORIF using small screws to manage the palmar comminution and keeping the articulation congruent. Also this approach allows for rapid active motion of the joint.
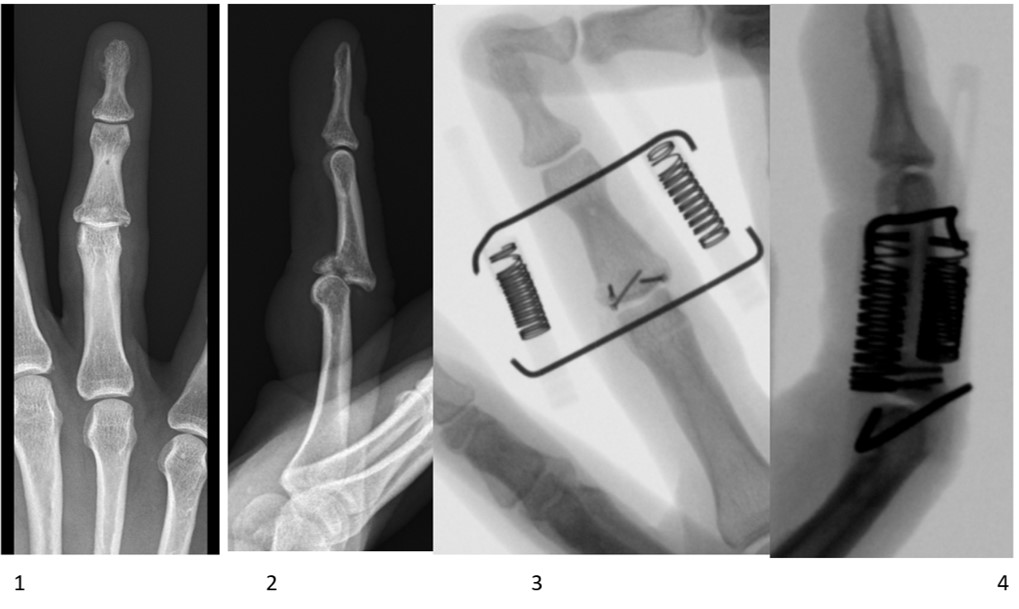

X-rays after external fixator removal ( 5 and 6) show good reduction and stability of the PIP joint. Arthroskopisch assistierte Behandlung von perilunären Luxationen
P. Boucke1, D. Merky1, C. Surke1, S. Hirsiger1, E. Vögelin1 (1Bern)
Show text
E: Chirurgisch werden verletzte Bänder und Frakturen bei perilunäre Verletzungen über einen offenen dorsalen und ggf. palmaren Zugang versorgt. Die Methode ist invasiv und hat oft eine erhebliche Bewegungseinschränkung zur Folge. Wobei sich diese, eben so wie die Faustschlusskraft in der Literatur bei einem follow-up >1 Jahr bei ca. 73%, respektive 76% der Gegenseite einpendeln. In den letzten Jahren wurden gute Resultate von rein arthroskopisch versorgten perilunären Luxationen publiziert. Vorwiegend stammen diese Arbeiten aus Asien, nur sehr wenige aus Europa. Wir gehen davon aus, dass die arthroskopische unterstützte Reposition zu einer geringeren Beeinträchtigung der Durchblutung und Narbenbildung führt, sodass unser Fokus seit einem Jahr auf der arthroskopischen Behandlung liegt.
M: Bei der arthroskopischen Versorgung erfolgt eine Inspektion der Verletzungen und ein Débridement der verletzten Bänder. Allfällige Frakturen werden perkutan versorgt und der Carpus mit perkutanen Kirschnerdrähten transfixiert. Postoperativ erfolgt eine Ruhigstellung im Scaphoidgips für mind. 8 Wochen. Nach anschliessender radiologischer Verlaufskontrolle werden die Drähte entfernt und mit Handtherapie begonnen. Weitere Kontrollen erfolgen 3 und 6 Monate postoperativ. Bestimmt wird der Bewegungsumfang in Flexion/Extension sowie Radial-/Ulnardeviation und die Faustschlusskraft, jeweils in % der Gegenseite.
R: In unserem Institut wurden seit September 2019 9 Patienten mit einer perilunären Luxation oder Luxationsfraktur behandelt. Darunter waren 2 minor arc Verletzungen (je 1x Mayfield Stadium 3&4) sowie 7 greater arc Luxationen, (6x Mayfield Stadium 3, 1x Stadium 4). Radiologisch zeigte sich ein guter Verlauf ohne vergrösserten SL Abstand oder zunehmende DISI Fehlstellung der proximalen Reihe verglichen zu den intraoperativen Aufnahmen. Dabei verbesserten sich die Flexion/Extension bis 6 Monate postoperativ von 66.8% auf 72.8%, die Faustschlusskraft von 54% auf 59%, wobei wir dies dem im Vgl. zur Literatur sehr kurzen follow-up zuschreiben. Der follow up betrug 3-9 Monate. Verzögerte Knochenheilung oder Pseudarthrosen traten in der Periode nicht auf.
D: Die vorläufigen Resultate der arthroskopischen Behandlung von perilunären Luxationen sind vielversprechend – die Patienten weisen eine günstige Heilung und im Seitenvergleich eine gute Bewegungsamplitude auf. Vorläufig konnte keine Verbreiterung des SL-Intervalles oder rasch progrediente Radiokarpalarthrose festgestellt werden.
Parosteal ossifying lipoma in the supinator muscle : about one case
L. Deghayli1, C. Bouvet1, N. Balagué1, P. Zaugg1 (1Sierre)
Show text
Case description: A right-handed patient presented with a slow-growing mass on the lateral side of her left elbow. She was referred to us due to paresthesia along the territory of the sensory branch of the radial nerve. The radiological workup reveals an ossifying mass within the supinator muscle with a peripheral fat density, suggesting an parosteal ossifying lipoma (see image) and we proceed with a surgical resection.
An antero-lateral approach along the supinator muscle allowed for en-bloc resection of the mass followed by neurolysis of the radial nerve and its sensory branch. The postoperative clinical course was favorable with the complete resolution of the paresthesia along the radial nerve. Pathology results confirmed the diagnosis of an paraosteal ossifying lipoma.
Discussion: Although lipomas represent by far the most common mesenchymal neoplasm, the parosteal lipoma is a rare entity often described in the literature as case reports. They are benign soft tissue tumors that can mimic malignancy like liposarcomas and that often present late as they are usually asymptomatic unless they compress adjacent structures, like in our case. They have been reported to occur most commonly in the femur, the tibia, the humerus and the radius. To our knowledge, there are no known cases of this pathology being found in the supinator muscle.

X-ray, CT scan and MRI showing the intra-muscular lipoma Sequenzielle Lappen in der Handchirurgie – Innovation oder nur Spielerei ?
C. Fritz1, E. Fritsche1 (1Luzern)
Show text
Einleitung
Eine der Möglichkeiten in der Lappenchirurgie zur Defektdeckung ist das Decken des Hebedefektes eines ersten Lappens mit einer zweiten Lappenplastik, die «sequential flaps method». Kann diese Methode auch in der Handchirurgie angewendet werden und ist sie auch sinnvoll oder doch nur «fancy-flap-surgery» ?
Methode und Material
Wir stellen 3 Fälle vor, bei welchen diese Technik angewendet worden ist. In einem Fall wird der Hebedefekt eines dorsalen Intermetacarpalelappens mit einem distal gestielten Interosseus anterior Lappen gedeckt. In einem zweiten Fall wird ein Perforator-Lappen des Grundgliedes eines Langfingers dorsal mit einem Intermetacarpale-Lappen gedeckt und in einem weiteren Fall wird der Hebedefekt eines Interosseous-anterior Lappens mit einem Interosseous-posterior Perforator-Lappen gedeckt.
Resultate
Alle 3 bezw. 6 Lappenplastiken sind sauber und ohne Komplikationen eingeheilt. Durch die «sequential-flap method» konnte verhindert werden, dass die Hebedefekt einer ersten Lappenplastik unter zu grosser Spannung verschlossen werden mussten bezw. dass keine Transplantate benötigt wurden, um Hebedefekte zu verschliessen.
Zusammenfassung
Die « Folge-Lappen-Technik» (um einen allerdings nicht offiziellen Terminus in deutscher Sprache zu wählen) ist durchaus auch in der Handchirurgie anwendbar und sinnvoll. Die guten funktionellen Ergebnisse müssen in Relation zu dem «Mehr» an Narben gesetzt werden. Diese Technik sollte allen Handchirurgen geläufig sein und ihre Indikation gehört zum Rüstzeug des Handchirurgen.
Kienböck disease after radius core decompression: correlates the radiological and clinical outcome?
M. Maniglio1, E. Zaidenberg2, S. Roner3, N. Habib4, G. Gallucci2, P. de Carli2 (1Lausanne; 2Buenos Aires AR; 3Chur; 4Lugano)
Show text
Introduction
For the treatment of Kienböck’s disease with distal radius core decompression, significant improvement in functional activity, motion and reduction of pain has been reported. However, in spite of these good clinical results, a radiological progression in a certain degree in the long-term follow-up is possible. Is there a negative correlation between the clinical improvement of the patients and the? Our study aims to figure out the correlation between the clinical improvement in Mayo wrist score and the radiological progression in the Lichtman classification in patients treated with core decompression for Kienböck’s disease.
Methods
24 patients (mean age: 38y; 10 women) treated with core decompression for Kienböck’s disease were included in this retrospective study. In 9 patients the dominant side was affected. The mean follow-up was 9.7 years (range, 3-18 years).
Clinical evaluation included preoperative and postoperative pain recorded using the visual analog scale, the active range of motion of the wrist in flexion and extension and the grip strength.
Subjective and objective clinical outcomes were assessed with help of the modified Mayo wrist score. We performed statistical correlation testing with the Spearman test.
Results
At end of follow-up 9 had an excellent result, 13 had a good and two a fair result. This was an average improvement of two levels in the Mayo classification. The pain was reduced by average 5.1 points in the VAS. The radiologic progression in the Lichtman classification was seen in 9 patients (five patients of one level, three patients of two and one patient of three levels). The Spearman correlation coefficient wasn’t significant: he was -0.056 between Mayo and Lichtman classification and 0.161 between VAS and Lichtman classification.
Discussion
Our results suggest, that there isn’t a clear correlation between the clinical and radiological outcome of patients after a distal radius core decompression in a middle to long-term follow-up. A radiological progression seems possible in the years after treatment, but patients keeps a satisfactory clinical outcome. In natural course of the Kienböck’s disease in elderly patients similar results were found by Taniguchi et al.
ConclusionThe clinical outcomes seem not to suffer in spite of a radiological progression in the Lichtman classification of patients treated with core decompression for Kienböck’s disease.
Is core decompression an effective treatment for Kienböck’s disease in middle-aged patients?
M. Maniglio1, E. Zaidenberg2, G. Thürig3, E. Gautier3, J. Boretto2, P. de Carli2 (1Lausanne; 2Buenos Aires AR; 3Fribourg)
Show text
Introduction
For the treatment of Kienböck’s disease, the distal radius core decompression provides the surgeon with a biologic-based technique that does not alter the anatomy of the radiocarpal, ulnocarpal, or radioulnar joints. Significant improvement in functional activity, motion and reduction of pain has been reported with this technique. However, a biological healing technique also needs a good healing potential. Since the regeneration potential deteriorates with the advancing age of a patient, we asked following question: Is a higher age associated with a poorer outcome and maybe a contraindication to this technic? Our study aims to compare the outcomes of patients with Kienböck’s disease, under and over 45 years old, treated with core decompression.
Material and Methods
36 patients treated with core decompression for Kienböck’s disease were included in this retrospective study. Patient were allocated to two cohorts according to their age at surgery. 22 patients (8 women) under 45 years old (mean: 28 y) were compared with 14 patients (8 women) 45 years old or older (mean: 52 y). The mean follow-up was 7 years (range, 1-18 years).
Clinical evaluation included preoperative and postoperative pain recorded using the visual analog scale, the active range of motion of the wrist in flexion and extension and the grip strength.
Subjective and objective clinical outcomes were assessed with help of the modified Mayo wrist score. We performed statistical comparisons using t-tests for parametric and the Mann-Whitney test for non-parametric data. Significance was set at less than .05.
Results
Preoperatively the mean VAS was 6.8 (range: 5-10) in patient under 45 years old and 5.6 (range,3-10) in patients over 45 years old. At the final follow-up the average VAS was 1.7 (range: 0-8) and 1.2 (range: 0-6) respectively. The improvement from preoperative to the end of the follow-up was significant in both groups (<45 years: p<0.001; >=45 years: p=0.003).
However, the difference between both age groups was neither significant preoperatively (p=0.075) nor postoperatively (p=0.445).
Also, in the other postoperative measurements (ROM, grip strength and Mayo score) there wasn’t any significant difference. However, from preoperative to postoperative the grip strength increased significantly in the younger age group (71% to 77%), but the increase of grip strength wasn’t significant in patients over 45 years old (72% to 80%).
Discussion
In this study a cohort of patients over 45 years old treated with core decompression for Kienböck’s disease were compared with a younger cohort. Similar clinical outcomes were showed, no matter to which age group patient belonged. Our results suggest that the radius core decompression is a simple, less invasive procedure that demonstrated favorable results also in a middle-aged patient cohort between 45 and 61 years old.
Conclusion
Core decompression should be considered as an important surgical alternative, also in middle-aged patients older than the “typical patient” with Kienböck’s disease.
Evaluation of Patient Satisfaction after Implantation of a Carpometacarpal Prothesis from 2017-2021
L. Dietrich1, I. Berner1, E. Blumer1, A. Behrndt1, C. Zimmermann1, U. Genewein1 (1Rheinfelden)
Show text
Background: Rhizarthrosis is a common degenerative disease of the aging population with increasing incidence. For years, trapezectomy was considered the undisputed gold standard for advanced rhizarthrosis. Advances in prosthetics made the innovative carpometacarpal (CMC) prosthesis available as an alternative. This surgical technique has been approved in Switzerland, but so far long-term results are still lacking. From our point of view, patient satisfaction postoperatively is of utmost importance.
Methods: Our clinic received approval for implantation of CMC prostheses in 2016. Since January 2017, 99 prostheses type ARPE were implanted. All 86 patients were included in the study. 13 (15.1%) patients have bilateral prosthesis. Patients were predominantly female (68.7%) with an average age of 70 years (39-83). The study includes 7 patients with known diabetes (8.1%) and 46 active smokers (53.5%). The ratio between the dominant and non-dominant upper extremity was 51:48. Complications occurred in 11 (12.8%) patients (luxation and/or ischemia). 6 patients underwent trapezectomy after implantation of a prosthesis. Satisfaction was defined as the sum of freedom from pain and functionality in daily life. We applied a standardized follow-up assessment. On a visual linear-analogue scale (VAS) from 0 (totally dissatisfied) to 10 (totally satisfied), patients rated their satisfaction with the prosthesis. All patients were asked whether they would have the procedure performed on the opposite hand or a hypothetical third hand.
Results: The satisfaction of the patients is at a mean value of 8.91 on VAS from 0 to 10. The 6 patients with trapeziectomy during the course of the study reported an average satisfaction of 6.5. Overall, 78 (90.7%) would undergo the surgery again if the opposite hand was affected, or on a hypothetical third hand. Compared with trapeziectomy, quicker postoperative recovery is shown in terms of pain duration and occupational therapy.
Conclusion: Our study shows that the satisfaction of patients after implantation of a CMC prothesis is very high (8.91 on VAS). In particular, the fact that the vast majority (90.7%) would choose surgery again on the opposite hand or on a hypothetical third hand shows the great potential of this technique. Furthermore, trapeziectomy is still possible after implantation of a prosthesis. These results support the innovative technique and explain the worldwide increase in implantations. Long-term results remain to be seen.
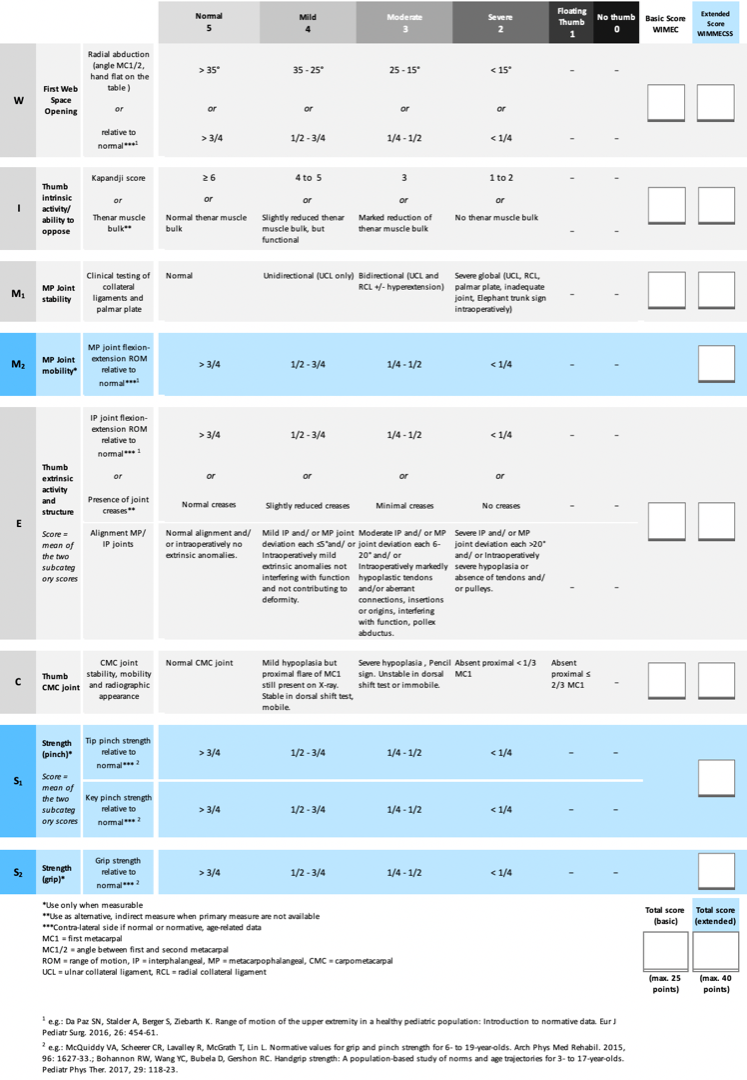
A functional assessment score for congenital hypoplastic thumbs
K. Mende1, M. A. Tonkin2 (1Basel; 2Sydney AU)
Show text
Background: For surgical reconstruction of congenital hypoplastic thumbs surgical techniques vary and the empirical evidence that allows for evaluation of the results is scarce. Uncontrolled, retrospective, descriptive studies with a low level of evidence are available. These vary considerably in terms of inclusion criteria, study populations, and the use of grading systems. Furthermore, the lack of standardized outcome measures prohibits a comparison of the results by means of meta-analyses and there’s a lack of standardized guidelines.
Methods: Based on our results from previous studies we developed a score that measures the specific anatomical anomalies as described in the Blauth grading, which is applicable in the very young and non-cooperative patient as well as in the older and cooperative one and allows for comparison of pre- and post-operative functional status as well as the results from different studies.
Results: A 5-category score based on the anatomical variations of the width of the first web (W), intrinsic function/ anomalies- ability to oppose (I), metacarpophalangeal (MP) joint stability (M), extrinsic function/ anomalies (E), CMC joint/ first metacarpal base (C), shown with the acronym WIMEC is proposed. The anatomical deficiencies in each category are scored from 5 (normal thumb) to 0 (absent thumb). To these anatomical variations are added three further assessment categories- MP joint mobility, strength of pinch, strength of grip, which are applicable for a more global functional assessment in cooperative patients. The full acronym becomes WIMMECSS. Strength and motion measurements are compared to the normal contra-lateral hand when possible, or with age-related normative values.
Conclusion: The thumb hypoplasia score (WIMEC) allows for an objective assessment and comparison of the pre- and postoperative status of hypoplastic thumbs, taking into consideration the anatomical deficiencies as described by Blauth, including intra-operative findings independently of the patients age and cooperation, and may therefore be used to evaluate the improvement gained from surgical reconstruction. The extended score (WIMMECSS) allows for evaluation and comparison of different techniques, for instance in the assessment of two types of opposition plasty, which may be used for comparison of results from different surgical units. The establishment of a multi-centre trial to determine the validity and any alteration in weighting of parameters is intended.
Suicide Attempt – Cardioplegic Solution - Migraine Surgery: Comprehensive care for a Hand Amputation
J. Bürgin1, A. Gohritz1, D. J. Schaefer1, K. Mende1 (1Basel)
Show text
Introduction: Hand macro-amputations require immediate treatment in a specialized centre by a trained team of microsurgeons. However, the success of the operation and its long-term outcome may not only depend on the replantation itself, but sometimes also need additional peri- and postoperative measures beyond anastomotic expertise, as presented in this exceptional case.
Case report: A 67-year-old male patient attempted to commit suicide because of chronic hemi-lateral occipital head-aches. Treatment was severely delayed for about 6 hours after the injury as the patient had hidden himself and the amputated hand in the forest. To prevent reperfusion injury, the hand had to be flushed by cardio-plegic solution and kept cold between admittance to the emergency department until the patient arrived in the operation room and vascular anastomosis could be started. The replantation could be completed after 7 hours, no postoperative complications occurred.
After several successful blocks of the left greater occipital nerve, in a second operation bilateral surgical nerve decompression in the neck was performed 17 months later. This revealed a severe greater occipital nerve entrapment by scar tissue on the symptomatic side, presumably due to work-related heavy loading and carrying on the left neck and shoulder for decades.
At 19-month after the replantation, the patient has regained a very useful hand function with good opening and strong grip which even enabled him to resume his original work as a plumber. Regarding the unbearable head-ache which made him suicidal, he is completely free of symptoms.
Conclusion: This case shows that beyond surgical performance during a macro-replantation, a holistic view and comprehensive treatment of the individual is important to achieve a successful long-term outcome.
Stability of the distal radioulnar joint with and without activation of forearm muscles
A. Weber1, L. Reissner1, S. Friedl1, A. Schweizer1 (1Zürich)
Show text
INTRODUCTION
The distal radioulnar joint (DRUJ) is not only crucial for the rotational movement in the forearm but also for power and load transfer. Torque movements and other activities that stress the wrist lead to physiological dorsovolar shift in the DRUJ complex.
Several studies have investigated this shift, and typical values (utilizing ultrasonography) were previously described. The primary aim of the present study was to examine the effect of the ulnar forearm muscles activation on DRUJ stability in healthy individuals. The primary outcome, therefore, was to measure the difference in dorsovolar ulna head translation in relation to the distal radius with and without activation of the ulnar forearm muscles (Flexor Carpi Ulnaris (FCU) and Extensor Carpi Ulnaris (ECU)).
METHODS
This study is a single-center, prospective, cohort study of otherwise healthy individuals (≥ 18 years, without history (or evidence) of pathology related to the DRUJ complex) who underwent a single examination and testing at our Institution. The study is powered to detect significant differences with N = 32 subjects. Enrollment began (April 2021) and is expected to conclude by August 2021.
The dorsovolar ulnar head translation in relation to the distal radius was measured in a transverse plane through the ulnar head and Lister tubercle. Measurements were carried out in the resting position and while the hand was actively pressed onto a surface (5 kg), with and without activation of the ulnar forearm muscles. Concurrently, an electromyogram was used to measure the FCU and ECU muscle activation.
RESULTS
Preliminary data on subjects (n = 4) thus far indicates an average total dorsovolar translation of wrists without muscle activation of 2.4 mm (SD = 0.95 mm). While ulnar forearm muscles were activated, the translation was only 0.8 mm (SD = 0.71 mm) on average. Muscle activation was monitored electrophysiologically, while the proportion of muscle activity (ECU vs. FCU) was similar (Root Mean Square = 153 mV vs. 151 mV).
DISCUSSION
Overall, our preliminary results indicate that ulnar translation with the activity of the ulnar forearm muscles is diminished by two-thirds compared to ulnar translation without the activity of these muscles. As such, ECU/FCU activation serve as additional secondary stabilizers of the DRUJ complex. This finding may be important as physicians discuss different treatment approaches for patients presenting with DRUJ instability.
-
08:30 – 18:00
Posteraustellung SGHR
Postoperative rehabilitation following CMC dual mobility prosthesis: a case study
A. Viola1, R. Stojmenova2, L. Priora1, I. Tami3 (1Mendrisio; 2Giubiasco; 3Gravesano)
Show text
Introduction
Carpometacarpal (CMC) osteoarthritis of the thumb basal joint is a very common and disabling condition that frequently affects middle-aged women and is a challenge for therapists.
If conservative treatment failed, many different surgical techniques could be proposed for this degenerative arthritis. Trapeziectomy with or without legamentoplasty is a gold standard treatment, instead total joint replacement with dual mobility prosthesis is relatively recent.
There are many studies about rehabilitation after trapeziectomy, but in literature we cannot find studies about rehabilitation regime after CMC prosthesis.
Case presentation report
A 44-years old woman with osteoarthritis of the first CMC joint (stage II, Eaton-Littler classification) started a conservative treatment with custom made splint for the night and joint protection education. The aim was to stabilizing the joint through muscle strengthening and gesture re-education.
Patient was been operated with a CMC dual mobility prothesis on the right hand (Touch, by Kerimed).
First day after surgery, early active motion protocol was started without any immobilization.
A CMC neoprene splint was worn for 6 weeks day and night.
1-2 weeks edema and wounds were managed, a gently active mobilization of the thumb started in all directions and pain-free. The patient was taught for home exercise in opposition, flexion, extension, adduction and abduction of the thumb and has been educated how to perform light activities of daily living.
3-6 weeks scar massage was begun, active and passive mobilization was performed to improve functional ROM.
For 6 weeks, no traction of the thumb and strength exercises to avoid prosthesis dislocations.
After 6 weeks, strengthening exercises was began, especially intrinsic and extrinsic thumb muscles.
Conclusion
In young women with osteoarthritis of the thumb, early mobilization seems to be an effective rehabilitation treatment after dual mobility CMC prosthesis.
Early return to activities of daily living, no pain, good pinch, fast strength recovery was indicated by the patient as characteristics of this rehabilitation.
Bibliography
Badia A., Total Joint Arthroplasty in the Treatment of Advanced Stages of Thumb Carpometacarpal Joint Osteoarthritis, J Hand Surg, 2006
Froschauer S., Total Arthroplastic with Ivory Prosthesis versus resection-suspension arthroplasty: a retrospective cohort study on 82 carpometacarpal-I osteoarthritis patients over 4 years, Europ. J of Medical Research, 2020
Bruner or Brunner? The Man Behind the Zig-Zag Incisions
E. Kulakli- Inceleme1, K. T. Danuser2, E. Fritsche1 (1Luzern; 2Zug)
Show text
Introduction
Finding the answer to Julian Minassian Bruner – or was it Brunner? His name is
mentioned almost daily in a routine workday of a hand surgeon and his zig zag incision
is a gold standard for the approach on the palmar side of the digits. But since decades
there has been an uncertainty about the way of writing Mr. Bruner’s last name.
Methods
To find the answer to this special and honorable name we had to go through the family
tree of Mr. Bruner’s ancestors. It is difficult to find data about the family tree of MD
Julian Minassian Bruner. But we found a book, “Our American Ancestors”, written by
Henry Lane Bruner and Elisabeth Bruner Taylor, the uncle and aunt of Julian M.
Bruner, written in 1943. Obviously, they themselves already were curious about their
family’s origin.
Conclusion
Literally - as sure as written in stone – the name of MD Julian M. Bruner is written with
one “N”. But looking at his family tree the origin of the name goes back to the
beginning of the 18th century with its roots in Germany. Johann Jacob Brun(n)er,
tracing Julian’s ancestors back seven generations, was born in Schifferstadt,Ludwigshafen, a town in the area of Rheinland-Pfalz in Germany and was the first
member to reach America. It was also the first member in the family tree where
documents have been found with the name Bruner written with two “N”s.
So - if someone nowadays writes the “Bruner Incision” with two N’s, they now at least
have a justification for their misspelling and rely on the origin of the name. But in
honor of MD Julian Minassian Bruner we suggest to simply follow his will, as it is
written on his grave, and continue writing “Bruner” with one “N”.
ROLE OF GRADED MOTOR IMAGERY IN PREVENTING CRPS AFTER SURGERY FOR DISTAL RADIUS FRACTURE
S. Pagella1, A. Viola2, L. Priora1, F. Ferrario1, M. G. Fioretti1, I. Tami1 (1Gravesano; 2Mendrisio)
Show text
Introduction: pain management is essential in the early stages of rehabilitation after surgery for distal radius fractures (DRF). Patients often are afraid to move the operated wrist, mainly because of pain. This might result in prolonged immobilization, resulting in stiffness and impaired function of the affected limb with devastating impact on working and social life. Pain becomes chronic in about 41.9% of the cases.It has been proved that pain in CRPS is associated with a reorganization of the primary sensory cortex with an alteration of the somatotopic cortical representation and loss of ability to integrate stimuli with spatial representation and discrimination between the affected and the healthy side. Motor performance is also compromised. Fortunately, these changes are not irreversible.The clinical application of these studies has seen the development of specific treatments that have as their objective the reduction of pain through a cortical reorganization and Graded Motor Imagery (GMI) is one of those. GMI is a form of brain training aimed to reduce pain and improved performance. It uses three stage approach: left-right discrimination, imaged movements and mirror therapy. We present a prospective and randomized study aimed to explore the ability of GMI to significantly reduce the incidence of CRPS in patient with DRF, after surgery.
Methods: We enrolled 60 consecutive patients with 60 DRF and we divided them in two groups. The allocation into these groups was randomized.In group A patients were treated in accordance with our standard protocol for DRF. In group B patients were treated with our standard protocol but also with GMI. We evaluated for statistical comparison all patients at 8 weeks postoperatively focusing on pain,Patient Rated Wrist Evaluation (PRWE), Brief Pain Inventory (BPI), McGill Pain Questionnaire MPQ. and function (ROM). We also recorded the presence of diagnostic criteria for CRPS.
Results:the number of simple medium severe or complicated fractures was similar between the 2 groups. At the last follow up patients in group B showed better results then patients in group A. This difference was not significant. There were 5 cases of CRPS in group A (without GMI).
Conclusions:our study suggests that GMI might implement standard rehabilitation protocols after surgery for DRS. GMI seems to have a protective effect against CRPS.
Skier’s thumb treatment with new orthosis and early mobilization
R. Stojmenova1, S. G. Rech2, T. Giesen3 (1Giubiasco; 2Lugano; 3Gravesano-Lugano)
Show text
Thumb ulnar collateral ligament (UCL) injuries are very common [1]. Conservative and post-operative regimes include immobilization of the metacarpophalangeal (MCP) joint for 10 days to 6 weeks [1-2], but, arguably, controlled early active motion stimulates healing of ligaments and avoid stiffness [3].
We treated 6 cases of UCL injuries (5 conservative, 1 post-operative) over a period of 2 months with a modified splint that allows early mobilization by protecting the torn ligament.
There were 3 women and 3 men with an average age of 42 years (range 29-52). One male patient was operated. We immobilized the MCP joint in a hand based splint (Figure 1) for 2 weeks. We then modified the splint by replacing the palmar block at the MCP joint with a velcro encouraging flexion of the MCP joint (Figure 2) for 4 weeks. The splint was still protecting radial and ulnar deviation while compensative flexion of the trapeziometacarpal joint was inhibited. The velcro was only removed during the exercises and light activities.
All patients eventually healed with good stability of the MCP joint; 90% of MCP flexion and Kapandji score of at least 9 was recovered at 8 weeks post injuries in all cases. Average Key Pinch was at 93% (range 5,5-10) at 8 weeks. This new regime seems to be safe with a fast recovery.
References:
- Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clin J Sport Med. 2010;20(2): 106-112.
- Harley BJ, Werner FW, Green JK. A biomechanical modeling of injury, repair, and rehabilitation of ulnar collateral ligament injuries of the thumb. J Hand Surg 2004;29(5);915-920.
- Michaud EJ, Flinn S, Seity WH Jr. Treatment of grade III thumb metacarpophalangeal ulnar collateral ligament injuries with early controlled motion using a hinged splint. J Hand Ther. 2010;23(1);77-82.


Das erste Lebensjahr eines Kindes mit Arthrogryposis multiplex congenita aus Sicht der Ergotherapie
M. von Gunten1, A. Ringeisen1 (1Bern)
Show text
Hintergrund
Arthrogryposis multiplex congenita [AMC] ist eine seltene Erkrankung mit angeborenen Gelenkkontrakturen, die unter anderem die oberen Extremitäten betreffen. Das erste Lebensjahr ist entscheidend, um Verbesserungen im Bereich der Körperstrukturen und –funktionen zu erzielen (Oishi et al., 2019). Durch die reduzierten Bewegungsfähigkeiten haben Neugeborene Mühe, ihre Arme zu heben und Gegenstände zu erkunden (Babik et al., 2020).
Ziel dieses Fallberichtes ist es, die ergotherapeutischen Massnahmen zur Unterstützung der Handlungsfähigkeit sowie Ergebnisse im ersten Lebensjahr eines Kindes mit AMC in den verschiedenen Bereichen der International Classification of Functioning, Disability and Health [ICF] vorzustellen. Zudem sollen Faktoren aufgezeigt werden, welche die Rehabilitation begünstigt und erschwert haben.
Fallbeschreibung
Die Interventionen beinhalteten unter anderem Schienenversorgungen, Mobilisation, Taping, Elektrostimulation, Adaptationen von Spielzeug sowie Beratung der Bezugspersonen. Das Mädchen besuchte die Ergotherapie ein- bis zweimal pro Woche. Die wichtigsten Ergebnisse waren eine Verbesserung der Gelenksbeweglichkeit sowie ein vermehrtes Nutzen der Hände zum Erkunden, Bewegen und Greifen von Gegenständen. Der Verlauf wird mit Bildmaterial und Verlaufsbeurteilungen dargestellt werden.
Begünstigende Faktoren waren eine vertrauensvolle Beziehung zwischen der Mutter und den Therapeut*innen und der interdisziplinäre Austausch. Erschwerend war das häufige starke und anhaltende Weinen des Mädchens, die Notwendigkeit, die Schienen häufig anzupassen und die limitierte Studienlage.
Schlussfolgerungen
Die Ergotherapie sollte früh begonnen werden und alle Komponenten der ICF berücksichtigen. Somit können Körperstrukturen und –Funktionen verbessert und die Eigenaktivität erhöht werden. Ein interdisziplinärer Austausch ist wichtig, um bei diesem komplexen Krankheitsbild Schwerpunkte zu definieren.
Babik, I., Cunha, A. B., & Lobo, M. A. (2020). Assistive and Rehabilitative Effects of the Playskin Lift TM Exoskeletal Garment on Reaching and Object Exploration in Children With Arthrogryposis. Am. Jour. of Occ. Ther., 75(1), 7501205110p1.
Oishi, S., Agranovich, O., Zlotolow, D., Wall, L., Stutz, C., Pajardi, G., Novelli, C., Abdel Ghani, H., Jester, A., Vuillermin, C., James, M., Manske, M. C., & Beckwith, T. (2019). Treatment and outcomes of arthrogryposis in the upper extremity. Am. Jour. of Med. Gen. Part C: Seminars in Medical Genetics, 181(3), 363–371.
New Desing for Scapula Winger's brace
S. Pagella1, F. Ferrario1, A. Viola2, T. Giesen1 (1Gravesano; 2Mendrisio)
Show text
Introduction: The most common causa of winging scapula (WS) is a close trauma to the long thoracic nerve and subsequent palsy of the serratus muscle.Initial treatment is mostly conservative, and includes the use of a splint designed to hold the scapula reduced on the chest wall. A reduced scapula, reduces pain and improves upper limb function while waiting for the serratus muscle to recover. If the palsy of the serratus persists, surgery is indicated. After surgery a similar splint is indicated. In literature it is longtime debated the difficulty in creating an equally effective and comfortable brace for WS. We present a new design for scapula winging splint we used in 4 patients pre and post operatively after long thoracic persistent nerve palsy. Methods: From June 2018 to February 2021 we treated 4 patients with post traumatic long thoracic palsy and consequent painful WS. The patients were all females with an average age 53 y.o. (range 23-76). All patients sustained a closed blunt trauma to the long thoracic nerve. All patients presented to our service with a long standing post traumatic scapula (>1 year). A WS splint was tailored before the operation and tested for 2 weeks before surgery. All patients underwent a transfer of the sterno-costal head of the pectoralis muscle to the tip of the scapula. Materials: a plate for the scapula area of thermoplastic material. Non-adhesive loop (NLV) Velcro, adhesive hook Velcro (AHV), Adhesive Padding, Soft velvet ending strip black. The thermoplastic material was molded directly on the patient's scapula. We introduced a border above the collarbone to strengthen the upper portion of the splint. We found how a perfect match of the lower part of the splint with the lower edge of the scapula is essential in maintaining the scapula reduced. The splint was was the completed with NLV and AHV very tight around the thorax just under the armpits and the breast. Original padding patterns were used around the lower part of the splint, posteriorly, were the most discomfort has been usually described. Splint was worn constantly above a normal t-shirt and removed carefully only to change clothes. Results: All patients recovered with the WS resolved and no residual pain. Al patients tolerated the splint adequately for all the pre and post operatively period.We think our modifications to the WS splint could be of use in this very specific pathology.
Martti V. et al, 2015
Marin R., 1998