Vendredi 28 novembre 2025, de 8h00 à 9h30
La session Gong Show est une série d’exposés attrayante, placée entièrement sous la devise « one case, one message ». Une présentation dure exactement 3 minutes, suivie de « Qu’est-ce que j’ai appris ? » (1 minute) et d’une brève discussion.
La discussion qui suit chaque présentation est animée par les chairpersons.
Les présentatrices et présentateurs (auteurs d‘abstracts) de cette session ne sont pas encore en possession du titre de spécialiste en chirurgie de la main (suisse ou étranger) mais ont l’intention de l’acquérir. La session Gong Show est réservée aux auteurs qui ont encore besoin d’une présentation au congrès SSCM pour obtenir le titre de spécialiste en chirurgie de la main. Un seul abstract par auteur est autorisé lors de la session Gong Show. La présentation de plusieurs exposés par le même auteur n’est pas possible.
Chaque année, la meilleure communication libre de la session Gong Show est récompensée par un prix.
NE MANQUEZ EN AUCUN CAS CETTE SESSION CAPTIVANTE!Vendredi 28 novembre 2025, de 8h00 à 9h30
Gong Show
|
08:15 – 09:30
|
Gong Show |
|
|
Saal A
Sessions SSCM
|
Lisa Reissner, Zürich CH; Thomas Mészáros, Villars-sur-Glâne CH
|
|
|
FMG1
Out-of-the-Box Arthroplasty: Transforming Trauma into Triumph
Fabienne Neff, Bern CH
AbstractObjective Methods Emergency surgery included revascularization of the small finger. The MCP joint injury of the ring finger was addressed with the implantation of a dual mobility implant designed for CMC I joint arthroplasty. The remaining radial collateral ligaments were reinserted. Active and passive mobilization began five days after surgery; no weight-bearing was allowed until ten weeks postoperatively. Results Discussion 
|
Langue(s)
|
|
|
FMG2
ATTR Amyloidosis in Hand Surgery: Current Status and Open Questions
Clara Marie Pecher, Zürich CH
AbstractBackground In amyloidosis, proteins misfold and aggregate in various tissues. In transthyretin amyloidosis (ATTR), misfolded transthyretin deposits in cardiac tissue, causing heart failure, conduction disorders, and cardiomyopathy. Previous studies suggest that symptoms such as carpal tunnel syndrome (CTS), trigger finger (TF), spinal stenosis, hearing loss, and biceps tendon rupture can be early signs of ATTR. ATTR occurs as wild-type (ATTRwt), common in the elderly, or as the rarer hereditary type (ATTRh). There is a wide range of genetic subtypes worldwide, each with distinct clinical manifestations. Bilateral CTS is observed in patients with ATTRwt and ATTRh. In the hereditary group, CTS often co-occurs with neuropathy, dysautonomia, and eye involvement. African American and Hispanic patients with the Val122Ile mutation often have more severe cardiac involvement and worse outcomes than those with ATTRwt. Aims We gathered data on ATTRwt and ATTRh subtypes and aimed to identify differences. We also re-evaluated biopsy size and tissue recommendations for Congo red stain in carpal tunnel and A1 pulley release. Methods We analyzed the literature and compared it to data collected at our clinic (May 2022-January 2023). A relatively low number of 3 out of 34 patients were ATTR-positive. We did not follow a diagnostic algorithm then. Therefore, we re-evaluated our patients for the presence of risk factors found in the literature. Since February 2023, we have performed biopsies in patients meeting these risk factors: bilateral CTS or TF in males >50y, females >60y. Results Among our 34 patients, 12 met the risk factors, 3 of these 12 tested positive, resulting in a positivity rate of 25%. Literature recommends a biopsy size >1cm2 of tenosynovium. Biopsy indication should be based on risk factors, not macroscopic findings. To date, we diagnosed 7 patients with ATTR, 5 underwent cardiological workup despite lacking clinical symptoms, 1 declined further workup, 1 is pending. Conclusions Long-term studies are needed to determine whether routine biopsies guided by clinical risk factors improve early diagnosis of ATTR. This depends on the likelihood of developing manifest ATTR after a positive biopsy. This study may have helped detect and possibly treat cardiac pathology even before clinical onset. Our recommendations on biopsy size (>1cm2 tenosynovium) and localization are consistent with existing literature and should be applied independently of macroscopic proliferation. |
Langue(s)
|
|
|
FMG3
Splinting beyond the limit: Overcorrection of a simple extensor tendon injury
Jakub Vaclavek, Aarau CH
AbstractIntroduction Tendinous mallet finger is a common pathology with a well-established protocol for conservative treatment. In this case we present a patient where the conservative treatment led to complications that required surgical revision and intense occupational therapy. Case Report We present the case of a 15-year-old male, who sustained a trauma to the pinky of his left hand playing handball. He was referred by the pediatric emergency department with a diagnosis of a tendinous mallet finger. Conservative management was initiated using a Stack splint for 8 weeks. Upon follow-up, the patient presented with a splint in extension, resulting in an hyperextension deformity (40°) of the distal interphalangeal (DIP) joint and a concurrent flexion contracture (15°) of the proximal interphalangeal (PIP) joint. The patient reported no pain and full finger flexion was present. Occupational therapy was initiated and a nighttime splint including the PIP joint was applied for another 8 weeks. While partial correction of the PIP contracture was achieved, the DIP hyperextension persisted. Clinical examination showed that the deformity was passively reducible. Sonographic evaluation demonstrated an intact central slip insertion with mild subluxation of the lateral bands. MRI was performed to further assess the extensor apparatus and revealed a shortened terminal slip. Surgical correction was recommended and accepted by the family. A WALANT tenolysis with Z-lengthening of the shortened terminal extensor tendon was performed. Postoperatively, the patient developed adhesions, resulting in limited DIP flexion. This was managed with intense hand therapy over 4 months. At the final 15 months follow-up, the patient demonstrated good flexion and extension of the digit, including complete fist closure. The range of motion in the DIP joint was extension/flexion 5/0/45°. Grip strength on Jamar Dynamometer revealed a symmetric strength of 45 kg. Conclusion This case highlights a rare iatrogenic complication of conservative mallet finger treatment. Immobilization in inadequate Stack splints can lead to a Boutonnière-like deformity. Surgical tendon lengthening and hand therapy restored full function. Early recognition and management are key to prevent permanent sequelae after accidental hyperextension splinting of finger joints. 
|
Langue(s)
|
|
|
FMG4
Conquering a Giant: Double-Barrel Fibula Reconstruction for Extensive Distal Radius Giant Cell Tumor
Julian Nachtsheim, Bern CH
AbstractIntroduction: Giant cell tumors of the bone present a significant challenge and often require complex reconstructive procedures, particularly in the upper extremity, to preserve both limb integrity and functionality. Materials and Methods: We present the case of a 28-year-old female patient diagnosed with a biopsy-confirmed giant cell tumor of the right dominant distal radius in May 2020. The initial treatment involved intralesional curettage, Argon beam therapy, defect filling with PMMA, and combined osteosynthesis. After a favorable initial outcome, the patient reported a new, tender swelling on the dorsal aspect of the distal radius nearly one year postoperatively, which was diagnosed as a recurrence. In response, a year-long systemic therapy with Denosumab was initiated, stabilizing the tumor. However, the development of radiocarpal and distal radioulnar joint (DRUJ) arthritis, compounded by partially intra-articular cement placement, led to significant pain and functional impairment, making the patient unable to work and prompting her to opt for a second surgery. Thus, two years postoperatively, in June 2022, after interdisciplinary consultation and 3D planning, reconstruction of the right distal radius was performed using a free, microvascular osteocutaneous fibula flap from the left leg, applied in a double-barrel technique with simultaneous RSL fusion. The sigmoid notch was reconstructed using an ipsilateral Brachioradialis tendon strip, while the Palmaris Longus tendon was used to repair the TFCC and extensor retinaculum. Results: Histological examination revealed clear bony and soft tissue resection margins. Seven months postoperatively, full consolidation of the fibula graft proximally and at the fibulo-lunate site was observed, with partial consolidation at the fibulo-scaphoid site. The patient's pain decreased rapidly and the range of motion and strength in her right wrist improved. At the most recent follow-up in May 2024, the patient expressed high satisfaction and reported no substantial limitations in her daily activities or professional life. There were no signs of local recurrence or lung metastases. Conclusion: Through complex bone and soft tissue reconstruction, this young patient’s destructive giant cell tumor of the right dominant radius was successfully treated curatively, despite recurrence, restoring a functional, pain-free limb.
|
Langue(s)
|
|
|
FMG5
A Search for the Best Outcomes in Scapholunate Dorsal Ganglions: Open, Arthroscopy, or Conservative?
Sabrina Hort, Winterthur CH
AbstractHypothesis Material and Methods Results
Conclusion |
Langue(s)
|
|
|
FMG6
Automated segmentation of fracture zones in distal radius fractures using deep learning methods
Prisca Alt, Schlieren CH
AbstractIntroduction: Numerous established classification systems for distal radius fractures and the corresponding surgical treatment strategies are based on the subdivision of intra-articular fractures into key fragments, which are separated by fracture lines or comminution zones. However, the morphology of the intervening fracture zones remains poorly understood. The aim of this study was to gain a deeper understanding of fracture zones in intra-articular distal radius fractures and to develop a deep learning-based method for the automated segmentation of these zones using computed tomography (CT) data. Methods: A dataset comprising 59 manually segmented and annotated CT scans of intra-articular distal radius fractures served as the ground truth. Fracture zones were algorithmically extracted from segmentations of individual bone fragments and were visually validated on a sample basis. A 3D U-Net was then trained to segment fracture zones in new CT scans. Various preprocessing steps, such as data augmentation, region-of-interest (RoI) cropping, and targeted modifications of the fracture zones, were implemented to optimize the model’s accuracy. Results: The best-performing model achieved a Dice score of 0.2944 and an Intersection over Union (IoU) of 0.1784 for the task of automated fracture zone segmentation. These comparatively low values were attributed to the challenges associated with generating a reliable ground truth dataset. Discussion: Fracture zones are often extremely difficult to delineate in CT scans, even for clinical experts, and frequently require interpolation based on professional experience during annotation. This contributes to a degree of uncertainty in the training data. Furthermore, the course of fracture zones follows a structural logic that is only partially discernible in CT imaging. Even fractures classified as identical can exhibit significantly different fracture zone morphologies. Conclusion: Overall, this study demonstrates that the automated segmentation of fracture zones remains limited at present and is subject to substantial methodological and data-related challenges. Nonetheless, a deeper understanding of fracture zone morphology through automated segmentation techniques could significantly enhance precision in diagnosis, classification, and surgical planning. 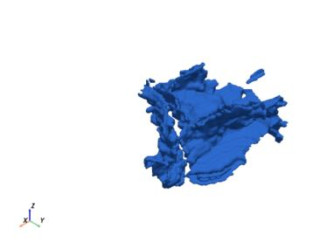

|
Langue(s)
|
|
|
FMG7
Attritional rupture of the Flexor Pollicis Longus Tendon by a Retrograde Scaphoid Screwing
Mélina Roulet, Fribourg CH
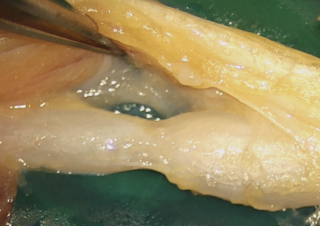
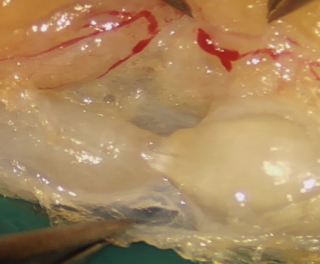
AbstractIntroduction: Attritional rupture of the flexor pollicis longus (FPL) tendon has been described in cases of friction on a palmar distal radius osteosynthesis plates. We present a case of an attritional rupture of the FPL tendon by a retrograde scaphoid screw inserted two years earlier. Commonly accepted surgical therapy of attritional tendon rupture is tendon reconstruction or tendon transfer. In this particular case a primary suture was performed. Materials and Methods: A 43-year-old high-level rock climber suffered a displaced fracture of the middle third of the scaphoid. The pre-operative ct scan revealed a bone cyst in the distal part of the scaphoid (Figure 1A). Due to this cyst, the retrograde Herbert like screw was inserted close to the palmar cortex to have the best hold in the bone (Figure 1B). Fracture healing was achieved after 6 weeks and the post-operative follow up remained unremarkable without any patient complaint. Two years later during an inverted grip in climbing (finger and thumb flexion with wrist hyperextension), the patient experienced a rupture of the FPL tendon due to palmar overhand. The palmar radiocarpal joint capsule was perforated (Figure 2). The screw protruding from the palmar surface of the scaphoid was removed. The FPL rupture was oblique and acute in appearance. Contact between the two stumps was easy and did not induce excess flexion of the thumb, which is why we opted for a direct suture and not an intercalated graft. Direct suture of the FPL tendon was performed using the Lim-Tsai technique (Supramid) and reinforced with a Krakow suture (FiberWire). Results: At three months post-operatively, the thumb's range of motion was almost complete : MCP flexion/extension was 40-0-0° (50-0-0°) and IP flexion/extension was 70-0-0° (70-0-0°). Wrist flexion/extension was 60-0-60° (70-0-70°). The patient resumed climbing at six months post-operatively. Conclusion: A retrograde scaphoid screw with palmar overhang is a risk for attritional FPL tendon rupture. Even asymptomatic retrograde screw with palmar overhang should be removed. Attritional tendon rupture with limited attritional zone can be sutured primarily. 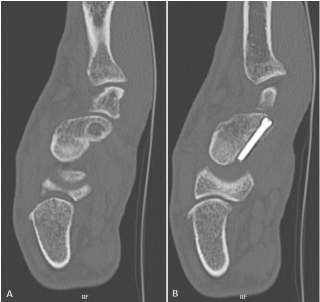

|
Langue(s)
|
|
|
FMG8
Hourglass like constriction of the posterior interosseous nerve : about a case
Damien Coppey, Orsières CH
AbstractIntroduction : Hourglass like constriction (HLC) is an uncommon spontaneous mononeuropathy that is typically characterised by a sudden onset of pain followed by palsy. The origin of this disorder remains unclear and the rarity of the condition makes its diagnosis difficult and its management uncertain. We report the case of a man who presented with acute left fingers drop due to HLC of the posterior interosseous nerve (PIN). Microneurolysis was performed after 6 months of conservative management without clinical evidence of recovery. Our hypothesis is that microneurolysis is an effective procedure for treating patients with radiologically confirmed HCL.
Material and methods : We report the story of a 34 years old patient, who presented acute non-traumatic pain centered on the left forearm, non-responsive to oral medication (NSAID, Paracetamol) which lasted 48h and ended with a complete loss of fingers extension and weakness of wrist extension with radial deviation. The pain was radiating in the arm and shoulder and associated with burning sensation or electric shock without allodynia. The patient was quickly addressed to a neurologist who conduct an ENMG exam which describes a focal motor neuropathy of the PIN. An echography done in the same time found and hourglass like constriction of the PIN 3cm distal to the elbow. After 4 months of physiotherapy, ergotherapy and electrical muscle stimulation, the clinical evaluation and the successive EMG exam were showing no evidence of recovery. In this setting microsurgical epi/perineurolysis was performed while taking care of preserving the axonal continuity.
Results : 2 months post operatively the patients was showing clinical evidence of recovery with wrist extension increasing from M4 to M5 and finger extension increasing from M0 to M2. Control EMG was not yet performed and will be repeated at 3 and 6 months after neurolysis.
Conclusion : Our conclusion is that microsurgical epi/perineurolysis is an effective procedure in the setting of HCL. Further follow up is still needed to confirm that hypothesis. Literature review confirmed that operative treatment gave better results than conservative treatment in patients with HCL.
|
Langue(s)
|
|
|
FMG9
Correction of rheumatoid thumb deformity by modified extensor pollicis longus rerouting technique.
Thomas Orthmann, Lausanne CH
AbstractAbstract
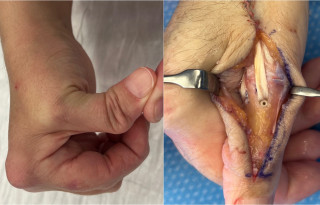
Introduction Chronic synovitis of the firtst metacarpophalangeal (MP) joint stretches out the dorsal capsule, extensor pollicis brevis tendon (EPB), and ulnar collateral ligament, leading to a characteristic deformity involving MP joint flexion, metacarpal adduction, and medial instability of the MP joint. Hyperextension or instability of the interphalangeal joint (IP) is often associated. The aim of these 2 cases is to present a modified surgical technique to treat the deformity.
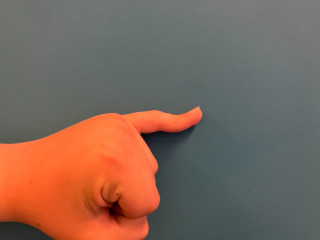
Material and methods We present 2 patients with rheumatoid thumb deformity that have been treated using the modified extensor pollicis longus (EPL) rerouting technique. The EPL was split longitudinally and divided distally. Synovial tissue surrounding MP joint was excised. A transosseous tunnel was drilled from dorsal to ulnar at the base of the proximal phalanx, through which the EPL was passed. Tension was adjusted to maintain the MP joint in 10° of flexion and fixed with a 2.5 mm interference screw inserted dorsally. The remaining EPL tendon was then secured on the ulnar side of the metacarpal head to reconstruct the ulnar collateral ligament (see Figure).
Results Complete IP joint range of motion was preserved in one case due to the insertion of the EPB on the distal phalanx. At 6 months after surgery, both patients were pain-free with no residual MP joint instability and demonstrated good first web space opening, improved pinch strength and increased MP joint range of motion.
Discussion Surgeons should be aware that the insertion of the EPB on the distal phalanx is more common in patients with rheumatoid thumb boutonnière deformity than in the general population (Okita et al., 2019). The proposed technique was inspired by the EPL rerouting method in boutonniere deformity (Nalebuff, 1984) and by procedure combining reconstruction of the ulnar collateral ligament of the MP joint of the thumb with restoration of opposition (Su et al., 1972). The modified technique restores both active extension and stabilizes the MP joint of the thumb.
|
Langue(s)
|
|
|
FMG10
Why 'Adelmann' Should Be 'Heister-Adelmann' and Favored Also for Ray II Procedures
Matteo Meroni, Luzern CH
AbstractIntroduction Recent publications see the controversy between primary and secondary transmetacarpal resection (also known as the “Adelmann” operation) versus finger amputation at the level of the proximal phalanx in favor of the transmetacarpal resection in the case of a functionally disturbing basal phalanx stump or, for aesthetic reasons. The available publications do not differentiate significantly between the resections of the rays II-V. This paper examines cases of II ray resections and presents the results. It will be checked whether the results agree with the current literature. Material and method We compiled 7 cases of primary and secondary ray resections (3 primary/4 secondary) of the II ray at the mid-metacarpal level and examined the long-term results in regards of function, including loss of strength in strength grip and fine grip, and pain. The results are presented. Results: The loss of strength in the transmetcarpal (II ray) amputee hands was on average 30% for both the strenght grip and the fine grip. Relevant neuroma pain was evident only in one of the cases. All patients would have the procedure performed again. The results are in good agreement with the, albeit sparse, literature. Discussion: In the past, transmetacarpal resections were often not recommended because the procedure may lead to a greater loss of hand strength than finger amputation at the level of the proximal phalanx. Our follow-up study in isolated cases with ray II resection cannot confirm this belief. The loss of strength was on average 30% for different grip types and is therefore of the same order of magnitude as the loss of strength reported in the literature for isolated index finger amputation at the level of the proximal phalanx. We can therefore recommend transmetacarpal resection in both primary and secondary cases, such as Adelmannn did already in 1852. However, Adelmann himself never performed this procedure for ray II, but he only recommended it. Moreover, Adelmann wrote in his paper in 1882, that the first description of this kind of operation must be attributed to Lorenz Heister and therefore the operation should be called “Heister-Adelmann” operation. 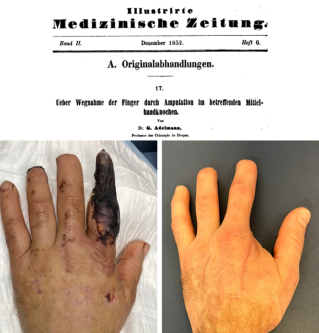
|
Langue(s)
|