Un grand merci à nos sponsors Or+, Or et Argent :
Jeudi
|
08:00 – 08:45
|
Enregistrement |
|
|
Break
|
||
|
08:30 – 09:00
Saal A
|
Ouverture conjointe
Ivan Tami, Lugano; Ursula Osterwalder, Baden
|
|
|
Joint Sessions SSCM / SSRM
|
||
Tendre la main pour guérir le système : une approche diplomatique de la politique de la santé
Raymond Loretan, Nyon
|
Langue(s)
|
|
|
09:00 – 09:15
Saal A
|
Présentation du Golden Hand Award
Daniel Herren, Zürich
|
|
|
Golden Hand Award-Sessions
|
Langue(s)
|
|
Vorstellung The Golden Hand Award
Daniel Herren, Zürich
|
||
|
09:30 – 10:30
Saal B
|
Communications libres I
Julie Dziwornu, Aarberg; Chiara Regotz, Naters
|
|
|
Sessions SSRM
|
||
|
FM60
Treatment of a Patient with Humerus fracture, Radial Nerve Lesion and CRPS : A Case Study
Matteo Malacrida, Como IT
AbstractIn this case study is exposed the care of a middle-aged patient who received arm trauma with humerus fracture and radial nerve injury. The case is complex, given the delay in taking charge by a hand therapist and due to comorbidities including CRPS. The patient presented at the first valutation a serious clinical picture:
The presentation will guide from the patient's admission three months after the operation with a severe disability (Quickdash 97/100 and PRWHE of 99/100). The functional aspects, limits during ADL, joint mobility and strength have been considered periodically (every two months) with datas and validated rating scales including Quickdash scale, Patient rated wrist/hand evaluation and 9 Holes. Adaptation of therapy and splints during the healing phases will be exposed with reference tables and images. The presentation will follow the therapeutic choices and the adaptation of therapy and splints manufacturing with the improvement of symptoms and reacquisition of mobility, functionality and strength of the upper limb up. The discussion will reach to the patient's reintegration into work, currently a watchmaker at 50% with an improvement at 46/100 for the Quickdash and 42 /100 for the PRWHE. Informed consent was signed on the collection of data and their use with exhaustive explanations on the procedure, purpose and destination of the case study. 


|
Langue(s)
|
|
|
FM61
Verlaufsorientierte Dokumentation der Nervenerholung mit dem Rosén-Score: ein Fallbericht
Iris Schütz, Zürich
AbstractContexte : Les lésions complexes des nerfs périphériques entraînent une perte de la sensibilité, des limitations de la motricité ainsi que de fréquentes douleurs telles que l’hyperesthésie et l’intolérance au froid. Cela affecte considérablement la fonction de la main et les activités quotidiennes des personnes concernées (1). Une évaluation structurée est essentielle pour planifier des mesures thérapeutiques ciblées et documenter l'évolution de la régénération nerveuse (2). Le Rosén-Score offre à cet effet un instrument standardisé permettant d'évaluer de manière exhaustive la sensibilité, la motricité et les troubles associés à la douleur. Objectif : L’utilisation du Rosén-Score pour une évaluation structurée et une documentation de la régénération nerveuse est présentée et expliquée à travers un exemple concret illustrant une lésion complexe du nerf médian. Méthodologie : L’impact fonctionnel et le déroulement de la régénération sont illustrés par une étude de cas. Les résultats ont été recueillis à intervalles réguliers et représentés graphiquement à l’aide du Rosén-Score. Les différentes évaluations ont été complétées par des enregistrements vidéo et des photos. Résultats/implication pour la pratique : Le Rosén-Score permet une évaluation différenciée et orientée sur l’évolution de la récupération fonctionnelle ainsi que sur les résultats après une suture des nerfs médian ou ulnaire à la hauteur du poignet ou de l’avant-bras distal. Il convient aussi bien à la documentation scientifique qu'à la pratique clinique quotidienne. Littérature
|
Langue(s)
|
|
|
FM62
Unusual nerve compression from a surgical and therapeutic point of view
Patricia Kammermann, Bern; Lena Fuest, Bern
AbstractContexte La fracture de l’hamulus ossis hamati est une lésion rare et souvent négligée. En raison de sa proximité anatomique avec le rameau profond du nerf ulnaire, une fracture peut provoquer une irritation ou une compression dans la loge de Guyon. Cela peut causer un déficit moteur, en particulier une faiblesse de la musculature intrinsèque, entraîner une perturbation de la motricité fine ainsi qu’une possible déformation en griffe des quatrième et cinquième doigts. Objectif L’objectif de cette étude de cas est de faire prendre conscience d’un lien potentiel entre une fracture de l’hamulus et une neuropathie ulnaire. Il s'agit notamment de souligner qu’en cas de déficit moteur isolé du nerf ulnaire sans déficit sensitif, il convient de rechercher spécifiquement une origine osseuse. Méthodologie En août 2024, un patient âgé de 21 ans a fait une chute à vélo sur sa main gauche. L’évaluation post-traumatique montrait une perte d’extension indolore de l’articulation PIP des doigts 4 et 5. Une radiographie conventionnelle a d'abord permis d'exclure une fracture, puis une échographie a permis d'écarter une lésion tendineuse. Près de trois mois plus tard, une atrophie au niveau du premier interosseux dorsal était visible cliniquement. Plus tard, une tomodensitométrie a révélé une fracture à la base de l'hamulus ossis hamati. Sur le plan thérapeutique, le patient a tenté de renforcer sa musculature intrinsèque à l’aide de l’électrothérapie ainsi que de maintenir la mobilité passive de ses articulations digitales. Des stratégies pour gérer le quotidien lui ont également été enseignées. Quelques semaines après la neurolyse et l’ostéosynthèse de l’hamulus ossis hamatum, la fonction du nerf ulnaire s’est totalement rétablie. Résultats Un déficit moteur du nerf ulnaire peut être dû à une fracture non diagnostiquée de l’hamulus ossis hamati. De petites nuances dans l’anamnèse et l’examen clinique font ici toute la différence et peuvent contribuer, grâce à la collaboration entre le chirurgien et le thérapeute de la main, à établir rapidement un diagnostic afin de lutter de manière ciblée contre l'atrophie musculaire. Une collaboration étroite et une communication directe entre la chirurgie et la thérapie de la main sont indispensables. Littérature
|
Langue(s)
|
|
|
09:30 – 10:30
Saal A
|
Session principale IUncommon Upper Extremity Nerve Compression: When to Think About it and What to Do
Moritz Hess, Olten; Laurent Wehrli, Lausanne; Florian Früh, Aarau
|
|
|
Joint Sessions SSCM / SSRM
|
||
Introduction
Florian Früh, Aarau; Laurent Wehrli, Lausanne
|
Langue(s)
|
|
Neurology
Andreas Schiller, Zürich
|
Langue(s)
|
|
Imaging
Roman Guggenberger, Winterthur
|
Langue(s)
|
|
Hand Therapy
Emanuele Mauri, Gravesano
|
Langue(s)
|
|
The irritative carpal tunnel syndrome
Francisco Del Piñal, ES
|
Langue(s)
|
|
Conclusion |
Langue(s)
|
|
|
10:30 – 11:00
|
Pause café |
|
|
Break
|
||
|
11:00 – 11:15
Saal A
|
Questions d’examen EBHS
Maurizio Calcagni, Zürich
|
|
|
Golden Hand Award-Sessions
|
||
EBHS-Prüfungsfragen |
||
|
11:00 – 12:30
Saal C
|
Communications libres IRadius and Wrist
Cesare Fusetti, Bellinzona; Christian Wirtz, Chur
|
|
|
Sessions SSCM
|
||
|
FM1
Lessons learned: 20 MOTEC® over 4 years
Léonie Hüsler, Luzern
AbstractEinführung Methodik Ergebnisse Schlussfolgerung |
Langue(s)
|
|
|
FM2
Isoelastic Resurfacing Prosthesis (Prosthelast®) for Comminuted Distal Radius Fractures
Ramon Damian Buechel, Sankt Gallen
AbstractIntroduction: Patients and Methods: Results: Conclusion: |
Langue(s)
|
|
|
FM3
Recovery After Total Wrist Arthroplasty: 1-Year Pain, Function, and Satisfaction Outcomes
Inga Besmens, Zürich
AbstractIntroduction: Traditional wrist fusion for painful osteoarthritis presents unsatisfactory trade-offs between pain relief and functional preservation. The Motec wrist prosthesis offers a technological advancement with its cementless, modular ball-and-socket design, yet comprehensive outcome analyses combining objective measures and patient-reported outcomes remain limited. Methods: This observational cohort study evaluated 22 patients (9 men, 13 women; mean age: 62 years) who underwent Motec wrist arthroplasty between March 2020 and March 2024. Outcomes were assessed preoperatively, at 3 months, and 12 months postoperatively using Numeric Pain Rating Scale (NPRS), Patient-Rated Wrist/Hand Evaluation (PRWHE), Total Active Motion (TAM), grip strength, and patient satisfaction measures using the outcome registry SUPEXOR. Results: Significant pain reduction occurred at both rest and during loading (p<0.05). PRWHE scores improved progressively across all time intervals (p<0.05). TAM showed delayed improvement, with significant gains between 3 and 12 months (p<0.05). Grip strength significantly improved from baseline to 12 months (p<0.05). At 12 months, 77% of patients reported high satisfaction, and 100% would undergo the procedure again. Discussion: Results demonstrated distinct recovery trajectories: pain improved rapidly, while motion and strength followed delayed patterns, informing rehabilitation protocols and patient counseling. Conclusion: Motec wrist arthroplasty provides significant pain relief and functional improvement with high patient satisfaction at one-year follow-up. |
Langue(s)
|
|
|
FM4
A decision-making algorithm for wrist arthroplasty in distal radius fractures in elderly patients
Massimo Sammons, Gravesano
AbstractComplex distal radius fractures (DRFs) in elderly patients are often complicated by osteoporosis and reduced bone density. This study examines the treatment of such fractures using wrist arthroplasty and presents our decision-making algorithm, which takes into account fracture morphology, patient age and needs, and associated wrist conditions.
Twenty-two patients with complex DRFs were treated between September 2020 and January 2025. The cohort included 4 males and 18 females, with a mean age of 75 years (range: 63–89 years). Fractures were classified using the AO system, and associated injuries were identified through radiographic assessments (X-rays and CT scans) in order to determine individualized treatment strategies. Patients who met the criteria of our algorithm underwent wrist arthroplasty and were followed up at 6 weeks, 3 months, and 6 months, including radiographic monitoring of implant osseointegration. Subsequently, patients completed the DASH (Disabilities of the Arm, Shoulder, and Hand) questionnaire and the PRWE (Patient-Rated Wrist Evaluation) test.
Our study reports satisfactory recovery of mobility (mean E/F 41-0-38°, P/S 64-0-66°) and grip strength (measured with the Jamar dynamometer, average of 16 kg). DASH and PRWE scores were comparable to current literature, considering the age of our study population.
Our study supports the effectiveness of Motec wrist arthroplasty as a viable treatment option for complex DRFs in a selected patient population, as determined by our decision-making algorithm. In future clinical scenarios, we aim to extend the follow-up period and increase the sample size. 
|
Langue(s)
|
|
|
FM5
Intercarpal kinematics after open surgical treatment for perilunate injuries
Mathias Häfeli, Chur
AbstractIntroduction: Perilunate dislocations (PLD) and fracture dislocations (PLFD) lead to a disruption of intrinsic and extrinsic ligaments of the wrist. The treatment includes open or arthroscopically assisted reduction, temporary transfixation of the carpal joints with or without ligament repair, and fracture fixation. Timely treatment and restoration of carpal alignment, can lead to satisfying clinical outcomes. Nonetheless, some restriction of range of motion and grip strength can be expected. While there is some literature on intercarpal kinematic changes after scapho-lunate injuries and scaphoid non-union, only little is known about these more complex injuries. Aim: To investigate intercarpal scaphoid and triquetrum motion in relation to the lunate and to compare this to the healthy wrist in patients after surgical treatment for PLD or trans-scaphoid PLFD. Material & Methods: 6 patients after PLD and 7 patients after trans-scaphoid PLFD underwent 4D-CT scans of the affected and the healthy wrist. During 4D-CT scanning, they actively performed a guided E-F and R-U motion. The difference in the radio-scaphoid (RSA) and radio-lunate angles (RLA) in neutral wrist position between affected and healthy side was measured. The smallest and largest distances in the SL-and the LT-joint within the motion cycle were determined as a measure of joint stability. Results: Mean follow-up after surgery was 94months (26-166). The difference in the RSA and RLA in neutral position between affected and healthy side was 10.1° (2.9°-26.7°) and 8.2° (0.9°-25.2°). There was no statistically significant difference between PLD and PLFD group. Scaphoid sagittal plane rotation during E-F showed a similar pattern in the affected and healthy wrist but the differences in the other planes were larger. Axial plane scaphoid translation during E-F showed small differences while they were bigger in the other planes. The motion patterns during R-U by trend showed larger differences than during E-F. The motion patterns of rotation and translation of the triquetrum were close to normal in most cases. The maximal SL-distance during E-F and R-U was larger in the affected side (p=0.033). No differences were found for the LT-distance and between PLD and PLFD groups. Conclusions: The intercarpal motion pattern for the SL- and LT-joints was quite similar in the healthy and the affected wrists. This indicates good restoration of the intrinsic carpal ligaments even though the SL-joint showed some widening. |
Langue(s)
|
|
|
FM6
Simple Excision for Managing Proximal Pole Scaphoid Nonunion
Maria Larrea Zabalo, Barcelona ES
AbstractPurpose: Due to the biological, anatomical, and biomechanical characteristics of the scaphoid, treating proximal pole nonunion remains challenging. The location of the nonunion (proximal or distal to the dorsal apex) may influence its natural history. Based on this concept, patients with a proximal pole nonunion located proximal to the dorsal apex and maintaining an intact insertion of the dorsal scapholunate ligament (DSLL) in the distal fragment of the scaphoid may benefit from simple excision of the proximal pole. This study evaluates the clinical and functional outcomes of this treatment approach. Methods: A retrospective review was conducted on 11 patients who underwent proximal pole simple excision for proximal pole scaphoid nonunion. Postoperative outcomes were assessed using pain (VAS), Patient-Rated Wrist Evaluation (PRWE), Patient-Specific Functional Scale (PSFS), and EQ-5D. Patient satisfaction and return to work rates were also analyzed. Results: Postoperative pain, PRWE, PSFS, and EQ-5D scores improved after surgery. 10/11 patients were highly satisfied with the procedure. 10/11 returned to their previous occupational activities. 4 patients reported dorsoradial discomfort, but only one required surgical revision for radial styloidectomy. No radiological progression to a scaphoid nonunion advanced collapse (SNAC) pattern or other complications were observed. Conclusions: These findings support that proximal pole simple excision is a viable and relatively simple treatment for proximal pole scaphoid nonunion when the proximal fragment is non-viable and a competent DSSL remains inserted in the distal fragment. |
Langue(s)
|
|
|
FM7
13 SEVEN YEARS EXPERIENCE OF SCAPHOCAPITATE ARTHODESIS WITHOUT JOINT PREPARATION
Stefano Lucchina, Locarno
AbstractPURPOSE To assess the effect of scaphocapitate arthrodesis (SCA) on grip strength and wrist motion for patients with advanced stages of Kienbock disesase (KD) or avascular necrosis of the proximal pole of the scaphoid (AVNPPS) without joint preparation. METHODS A retrospective review was conducted of patients with advanced stages of KD (stage IIIB according to Lichtman classification) or avascular necrosis of the proximal pole of the scaphoid with a minimum of 1 year clinical follow-up. Outcome measures included preoperative and postoperative pain, range of motion, grip strength, complications, additional surgery, radiographic changes and the modified Mayo wrist score. RESULTS Twenty-two patients (21 males and 1 female) with a mean age of 34 years (range, 16-54 y) at the time of the SCA were included in the study. The mean follow-up period was 101 months (range 11-171 mo). The ave AROM of the wrist was 92.6°. The TAM ratio and Jamar ratio compared to the contralateral were 66.6% and 79.4% respectively. The Modified Mayo wrist scores were mostly fair (50%) being good and poor in 30% and 20% of cases respectively. All patients returned to regular employement. The ave time out of work was 4.6 months (range 2-15 mo.). Most patients had a marked improvement of the wrist pain that passed from 7.9 to 1.8 at the VAS-score. Neither progressive radiographic carpal collapse and ulnar traslocation of the carpus in case of KD occurred nor signs of SNAC wrist of panarthritis occurred. In 50% of cases a bone resorption in the capitate was detectable but It was not associated with the time of follow-up and with post-operative pain. One case of hardware malposition required a conversion to total wrist joint fusion. SUMMARY SCA resulted in clinical improvement in cases of advanced stages of KD and AVNPPS in medium-term follow-up even without preparation of the SC joint. No hardware related complications were observed, except in one case. SCA represents a valid salvage procedure in cases of advanced KD or AVNPPS. |
Langue(s)
|
|
|
FM8
Outcomes of Proximal Row Carpectomy and STT Arthrodesis in Kienböck’s Disease: A Meta-Analysis
Carl Flamin Meuth, Bern
AbstractIntroduction: Kienböck’s being a rare disorder, studies are underpowered to compare Proximal Row Carpectomy (PRC), Scapho-Trapezio-Trapezoid Arthrodesis (STTA), and Scapho-Capitate Arthrodesis (SCA). Complementing a recent meta-analysis focused on SCA (Bouri 2023), a comparison of clinical outcomes of PRC and STTA would thus be most desirable for surgeons and patients. Disclosures: |
Langue(s)
|
|
|
FM9
The inside-out Volar Midcarpal Direct Scaphoid portal: Anatomical study and technical recommendations
Maria Larrea Zabalo, Barcelona ES
AbstractIntroduction / Objective: Material and Methods: Results: Discussion and Conclusions: |
Langue(s)
|
|
|
FM10
Arthroscopic Reconstruction of Scaphoid Nonunion: Insights from 40 Cases
Dominique Nellie Merky, Bern
AbstractIntroduction: Scaphoid nonunions remain a common and challenging condition in hand surgery. With the advent of arthroscopy, bone graft reconstruction can now be performed using a minimally invasive, arthroscopically assisted technique. This study presents a series of 40 arthroscopically treated scaphoid nonunions, highlighting its adventage as a minimally invasive technique with excellent outcomes and potential for ambulatory implementation. Material and Methods: We retrospectively evaluated 40 patients (on average 30 yeras, age range: 12- 58 years) treated with an arthroscopic reconstruction of a scaphoid nonunion at our institution. All surgeries were performed by the same surgical team. Follow-up ranged from 2 months to 2 years. The technique included arthroscopic debridement, bone grafting, and internal fixation, using one or two headless compression screws. Cases were assessed clinically and radiologically, focusing on union rates, correction of deformity, surgical time, and complications. Results: Union was achieved in 38 of 40 cases (95%). In the two remaining cases, the proximal pole was significantly sclerotic both pre- and intraoperatively. Despite radiographic signs of persistent nonunion, both patients remained asymptomatic postoperatively. Importantly, no humpback deformities were observed in any case. Surgical time was significantly reduced compared to open techniques, and no conversions to open surgery were necessary. No infections or neurovascular injuries occurred. Discussion and Conclusion: Arthroscopic reconstruction of scaphoid nonunions offers a safe, effective, and minimally invasive alternative to open procedures. The technique preserves soft tissues, reduces operative time, and delivers excellent anatomical and functional outcomes. Even in cases where radiologic healing is incomplete, the clinical results can be satisfying. Given its low morbidity and efficiency, this technique is ideally suited for ambulatory surgical settings—should future healthcare frameworks allow for it. Based on our results, we strongly recommend this approach as a standard option for treating scaphoid nonunions. |
Langue(s)
|
|
|
FM11
Short- to mid-term results of the ANAFAB reconstruction for scapholunate instability
Katharina Richetti, Chur
AbstractIntroduction Delayed diagnosis of scapholunate (SL) ligament injuries limits therapeutic options and often prevents direct ligament repair, requiring ligament reconstruction. The anatomical front and back (ANAFAB) procedure for SL instability proposed by Sandow and Fisher combines the reconstruction of the scaphotrapezium (ST), dorsal scapholunate (SL), and long radiolunate (LRL) ligaments addressing several important parts of the SL complex. Methods We conducted a single-center, retrospective trial including all patients treated for SL instability with the ANAFAB procedure at our clinic. No exclusion criteria were applied. Procedures were performed by 3 different surgeons with level 5 expertise. We reviewed demographic data, pre- and postoperative (latest follow-up) range of motion (ROM), grip and pinch strength. We measured SL distance, scapholunate, radiolunate, and radioscaphoid angle (SL, RL, RS), carpal height and ulnar translation on standard radiographs. Patient-reported outcome measures (PROMs) were analysed if available. Results Between 2019 and 2025, 8 patients underwent the ANAFAB procedure for chronic SL instability. 1 patient had prior failed ligament repair. 1 had additional adaptive carpal instability from radial malunion and underwent corrective osteotomy in the same surgery. Male:female ratio was 6:2, median age at time of surgery 42.5 years (range 34 – 56), follow-up 24 months (3 – 55). Preoperative E/F was 60/60 (30/40 – 70/80, n = 5), R/U 15/25 (10/10 – 35/40), P/S 90/85 (60/75 – 90/95); grip strength was 27.5 kp (21 – 36, n = 4); SL distance 3.4 mm (1.8 – 4, n = 7); pain on a 10-point VAS (n = 3) was 4 at rest (1 – 4), 6 under load (6 – 8). Postoperative E/F was 61/45 (40/20 – 80/60, n = 6), R/U 17.5/30 (5/20 – 20/35), P/S 77.5/89 (60/70 – 90/100); grip strength was 36 kp (10 – 55, n = 7); SL distance 3.5 mm (2 – 4, n = 7); pain on VAS (n = 3) 1 at rest (0 – 3), 1 under load (1 – 6). 7 out of 8 patients returned to previous work. Conclusion In our small cohort, the ANAFAB procedure was effective in reducing pain allowing patients to return to daily activities and work. Although radiological results were not always satisfactory and some flexion was lost, we can expect preserved extension, improved strength and high patient satisfaction. Therefore, this technique currently remains our treatment of choice in these cases. Disclosures Conflicts of interest: none Informed consent: obtained Submission elsewhere: none |
Langue(s)
|
|
|
11:00 – 12:30
Saal B
|
Communications libres II
Rebecca Glanzmann, Sursee; Moritz Hess, Olten
|
|
|
Sessions SSRM
|
||
|
FM65
Von der Diagnose zur Effizienz: Retrospektive Analyse handtherapeutischer Assessments und Konzepte
Astrid Schmid, Thun
AbstractIntroduction : Compte tenu de la pénurie de personnel qualifié et du nombre croissant de patients, les cabinets de thérapie de la main sont confrontés au défi d’organiser efficacement des soins de haute qualité. Un aperçu des diagnostics les plus fréquents peut aider à développer des évaluations et des stratégies de traitement ciblées et liées aux activités quotidiennes. L’objectif de cette analyse rétrospective était de recenser l’éventail des diagnostics de notre cabinet de thérapie de la main ambulatoire et d’en tirer les conclusions pratiques pour le choix des évaluations et les protocoles de traitement. Méthodologie : Tous les cas traités entre janvier 2016 et mai 2024 ont été extraits de la documentation numérique et catégorisés par diagnostic. Les cinq diagnostics isolés les plus fréquents ont été déterminés. En parallèle, une réflexion a été menée sur les évaluations appropriées à ces groupes principaux et sur la manière dont elles peuvent contribuer à la promotion de l’autonomie et de l’efficacité. Résultats : Les diagnostics les plus fréquents étaient : 1) fractures du radius, 2) lésions des tendons extenseurs, 3) tendinopathies, 4) fractures des doigts (P1-3), 5) fractures MCP (D2-5). Pour ces diagnostics hétérogènes, la Single Assessment Numeric Evaluation (SANE) et la Patient-Specific Functional Scale (PSFS) ont été identifiées comme des instruments rapides à utiliser et ayant un lien avec la vie quotidienne (1,2). Les deux évaluations peuvent être remplies avec le patient pendant la séance, fournissent un feedback direct et permettent une adaptation ciblée du traitement. Sur la base de l'analyse des diagnostics, un nouveau protocole de traitement pour les fractures des métacarpiens a également été introduit en 2023, ce qui a entraîné une réduction significative du nombre de séances de thérapie par cas. Implication pour la pratique : La combinaison de l’analyse du diagnostic et du choix ciblé des évaluations fournit une base fondée sur des données pour des thérapies préservant les ressources et se concentrant sur le client. La SANE et la PSFS permettent une documentation rapide, favorisent la participation du patient et soutiennent un programme d’exercices à domicile structuré. L’accent mis sur les cinq diagnostics les plus fréquents restera central à l’avenir afin de développer d’autres protocoles de traitement pour une rééducation de la main efficace.
|
Langue(s)
|
|
|
FM66
Using Artificial Intelligence for Retrospective Analysis of Clinical Data in Hand Therapy
Lorenzo Negro, Chiasso
AbstractBackground and Objectives:
Results: Conclusions: |
Langue(s)
|
|
|
FM67
Reduce to the Max: From 37 to 4 questions in the Michigan Hand Outcomes Questionnaire
Kei Mathis, Zürich
AbstractIntroduction: The Michigan Hand Outcomes Questionnaire (MHQ) has been criticized for its length, with 37 questions across 6 subscales, making it time-consuming for patients to complete. This study aims to shorten the MHQ by developing an electronic decision tree (DT) version. Methods: MHQ scores were prospectively collected from 72'869 patients with different hand conditions at Xpert Clinics, the Netherlands. The mean age was 58 years, 59% were female, and the treatment was either surgical (71%) or conservative (29%). Using a Chi-Squared-Automatic Interaction Detection algorithm, separate DTs were created for each MHQ subscale and the MHQ total score. Additionally, the total score was calculated by summing the scores from DT versions of each subscale. We used 75% of the data for training and 25% for testing the developed models. We selected the DT for each subscale and for the total score with as few items as possible with the criteria that 1) the Intraclass Correlation Coefficient (ICC) with the original score was greater than 0.9 and 2) the median absolute error between the predicted and original scores was below the minimally important difference. Results: The number of questions for the total score decreased from 37 to 16 when calculated by summing the DT subscales, and from 37 to 4 when predicted by a separate DT. The number of questions for the DT subscales was reduced by 20% to 83% compared to the original questionnaire. The ICC between the original and predicted DT scores ranged from 0.92 to 0.99, with a median absolute error between 0 and 4.2 points. All scores were well below their respective minimally important differences. We created a free online tool to calculate the MHQ based on the developed algorithm. Conclusion: The 37-item MHQ could be reduced to 16 questions when all the subscales were determined and even to 4 items if only the total score was calculated, while maintaining high accuracy. This development is in line with current advances in patient-reported outcome measures which aim to shorten questionnaires and tailor them to patients using specific algorithms. This shorter version, accessible in an online tool, can improve usability, allowing more doctors to assess patients' health and tailor treatments to meet patients' needs. |
Langue(s)
|
|
|
FM68
MAT AssessTherapy App – Handbefundung digital auf den Punkt gebracht
Andrea Moser, St. Veit An Der Glan AT
AbstractUne thérapeute de la main s’est posé la question suivante : comment présenter les progrès réalisés en rééducation de la main de manière compréhensible, tangible et significative pour toutes les parties concernées, à savoir les patients, les médecins, les collègues et les organismes payeurs ? Cette idée a donné naissance à une fiche structurée sur laquelle documenter des paramètres tels que la force, la mobilité, la dextérité, la douleur et les fonctions en rapport avec la vie quotidienne, et de les représenter visuellement à l'aide des couleurs des feux de signalisation. Cette fiche a été testée dans la pratique quotidienne et évaluée à l’aide d’un questionnaire rempli par 300 experts en thérapie de la main. Les résultats ont été publiés dans ErgoScience. A la fin de l’article, une vision claire se dégageait : développer à partir de la feuille de papier une solution numérique, adaptée à un usage quotidien. Ce projet a été soumis en 2024 lors du Shark Tank de la FESSH à Rotterdam et a remporté la deuxième place. C’est ainsi qu’est née AssessTherapy : une application internet qui soutient le thérapeute dans la sélection de tests validés, calcule les moyennes automatiquement, représente les progrès de manière visuelle et crée une fiche de résultats structurée en un clic. Les patients bénéficient d’une présentation compréhensible et motivante de leurs progrès. Les thérapeutes gagnent du temps, ont une vue d’ensemble et disposent d'un moyen de documentation moderne. Ce projet n’a pas été encouragé par un groupe industriel ou une entreprise pharmaceutique, mais par des thérapeutes l’ayant eux-mêmes développés : sans lobby, mais avec leur expertise, leur passion et d’innombrables heures bénévoles. Parce qu’il est temps que la qualité thérapeutique soit mesurable, visible, et reconnue comme faisant partie intégrante des soins professionnels. C'est exactement ce que permet cette application : elle nous place au même niveau que les autres métiers de la santé, renforce notre identité professionnelle et s’adresse également à la prochaine génération de thérapeutes. Car rendre visible numériquement les effets de la thérapie ne modifie pas seulement la documentation, mais aussi l'image qu'a de lui-même tout un groupe professionnel. |
Langue(s)
|
|
|
FM69
Implémentation de la santé numérique en rééducation de la main via une application smartphone
Pauline Chèvre, Fribourg
AbstractLa santé numérique s’impose comme un pilier des politiques de santé à l’échelle mondiale, et son essor est encore plus significatif depuis la pandémie de Covid-19. En Suisse, son développement est soutenu par les stratégies nationales. C’est un moyen de garantir un accès aux soins équitable et abordable, notamment grâce aux thérapies à distance et aux applications mobiles. L’ergothérapie n’échappe pas à ce contexte. L’utilisation de la télésanté commence à faire ses preuves. Néanmoins, les facteurs personnels, le matériel et l’environnement peuvent être des barrières à la mise en place d’une telle approche.1 Le succès d’un outil numérique dépend donc de sa facilité d’utilisation mais également de la satisfaction du patient à recourir à une telle méthode.2 En 2025, notre hôpital a intégré l’application mobile PhysiTrack® dans la prise en charge de patients souffrant d'une lésion à la main. Cette application permet de créer des programmes d’exercices sous forme de vidéos, accompagnées d’explications orales et écrites. Nous en étudions actuellement la clarté didactique, la motivation et l’adhésion au traitement au moyen d’un questionnaire. Les premiers résultats, issus d’une dizaine de participants, indiquent une utilisation régulière de l’outil. Celui-ci est perçu comme pratique, attrayant et utile à la compréhension des exercices. Une évaluation sur un échantillon plus large est en cours pour vérifier cette tendance. Nos résultats intermédiaires indiquent que l’utilisation d’un support numérique en thérapie de la main est non seulement un complément au traitement en présentiel mais également une plus-value. La hausse des coûts de la santé et la pénurie de personnel fragilisent le système de soins. La télésanté constitue une réponse possible, en facilitant l’accès à l’ergothérapie sans compromettre la qualité de la prise en charge. D’autres recherches restent toutefois nécessaires afin d’approfondir cette thématique actuelle.
|
Langue(s)
|
|
|
FM73
Gemeinsam statt einsam: Gruppentherapie als frischer Impuls in der Handtherapie
Andrea Moser, St. Veit An Der Glan AT
AbstractLa guérison de la main nécessite parfois plus qu’une thérapie individuelle. Ce concept de groupe structuré s’adresse à un maximum de dix patients souffrant d’une blessure à la main – indépendamment du diagnostic ou des antécédents. Ensemble, ils bougent, rient, essaient et se renforcent. Les séances suivent une structure claire :
L’aspect social est au cœur du projet : les participants ressentent une connexion, un soutien mutuel et une nouvelle motivation. Les personnes ayant subi une amputation montrent à nouveau leur main pour la première fois. Les patients souffrant de douleurs bénéficient de l'exemple des participants plus avancés. Il s’agit d’un espace sûr, où le courage, l’acceptation et l'efficacité personnelle se développent. L’efficacité a été évaluée à l’aide d’un questionnaire et de l’application MAT-Hand. Cette dernière enregistre les paramètres pertinents pour la thérapie de la main tels que la force, la mobilité, la dextérité et la douleur et représente les changements de manière visuelle à l'aide des couleurs des feux tricolores. Le questionnaire visait à déterminer si les patients avaient perçu des progrès de la fonction de leur main grâce à la thérapie de groupe. Résultats : La thérapie de groupe a un effet sur la fonction, les émotions et la motivation. |
Langue(s)
|
|
|
11:15 – 12:30
Saal A
|
Special SessionArthroscopy in Wrist and Hand Traumatology: The Spain Experience
Martina Greminger, St. Gallen; Maurizio Calcagni, Zürich; Marianne von Haller, Pratteln
|
|
|
Joint Sessions SSCM / SSRM
|
||
Arthroscopy in Distal Radius Fractures and Malunion
Francisco Del Piñal, ES
|
Langue(s)
|
|
Arthroscopy in Scaphoid Fractures and Nonunion
Pedro J. Delgado, ES
|
Langue(s)
|
|
The role of Arthroscopy in Small Joint Fractures
Vicente Carratalá, ES
|
Langue(s)
|
|
Benefits of Arthroscopic Treatment of Wrist and Hand Injuries from a Therapeutic Point of View
Roberto Ucero Lozano, Madrid ES
|
Langue(s)
|
|
|
12:30 – 13:45
|
Lunch and Networking |
|
|
Break
|
||
|
12:45 – 13:30
Saal B
|
Symposium de midi 1 |
|
|
Symposium de midi
|
||
VOLT - Variable Angle Optimized Locking Technology
Frank Beeres, Luzern
|
||
|
12:45 – 13:30
Saal C
|
Symposium de midi 2 |
|
|
Symposium de midi
|
||
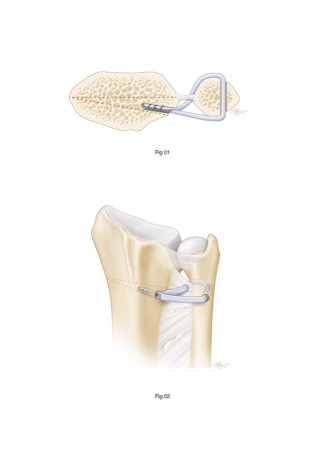
Rekonstruktion des skapholunären Bandes mit InternalBrace
Pascal Ducommun, Cham ; Giuseppe Broccoli, Winterthur
|
||
|
12:45 – 13:30
Saal A
|
Session Jeunes chirurgiens de la main Suisse
Mauro Maniglio, Zürich; Sophie Charlotte Brackertz, Zürich
|
|
|
Sessions SSCM
|
||
Welcome |
||
|
Bilan de l’année |
||
|
Election de la nouvelle/du nouveau Vice-Président/e |
||
|
L’amour est dans l’hôpital Deux centres de formation suisses se présentent
Alexandre Kämpfen, Basel; Ivan Tami, Lugano
|
||
|
13:45 – 14:30
Saal A
|
Narakas Lecture
Alex Lluch, Barcelona ES; Maurizio Calcagni, Zürich
|
|
|
Sessions SSCM
|
||
A journey through carpal instabilities
Alex Lluch, Barcelona ES
|
Langue(s)
|
|
|
14:15 – 15:30
Saal C
|
Communications libres IINerves
Alexandre Kämpfen, Basel; Jean-Yves Beaulieu, Genève
|
|
|
Sessions SSCM
|
||
|
FM12
Clinical Results of Motor Nerve Transfer from a Branch of the Triceps to the Axillary Nerve.
Emmanuelle Richard, Lausanne FR
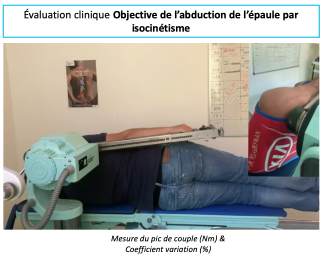
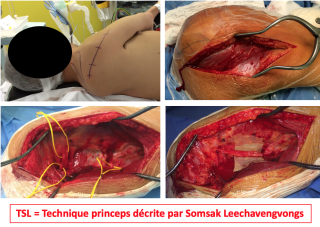
AbstractIntroduction : L’objectif de ce travail était d’évaluer les résultats cliniques et facteurs pronostiques de 12 ans d’expérience du transfert nerveux de la longue portion du triceps sur le nerf axillaire (TSL). Matériel et Méthodes : Cette étude rétrospective monocentrique, évaluait les patients opérés d'un TSL (2008-2019) avec un recul minimum de 18 mois. Les résultats étaient évalués globalement puis en sous-groupe soit TSL isolé (TSLi) contre TSL + autre transfert (TSL+). Les critère de jugement principal était l'échelle du test BMRC, les critères de jugement secondaies étaient la mesure des mobilités de l'épaule et un test isocinétique de l'abduction. Un deltoïde moyen (DM) DM M3 ou plus sur l'échelle BMRC témoignait d’une récupération. Résultats : Trente-six patients étaient inclus avec un recul moyen de 47 ±4 mois, âgés de 28 ans (15-68) et opérés à 8 mois post-traumatique (4-28). On retrouvait un Deltoïde supérieur ou égal à M3 pour 72% de deltoïdes antérieurs, 75% de moyens et postérieurs. Les mobilités augmentées étaient l'élévation antérieure et l'abduction (+35 et +55°, p=0,003). Le pic de couple était significativement diminué en concentrique par rapport au côté sain de -30% à 60°/s, de -31% à 180°/s, et de -26% en excentrique à 30°/s (p<0,001). Les résultats en force et mobilités étaient supérieurs pour le groupe TSLi. Les facteurs pronostiques significatifs étaient : TSL + autre transfert (p=0,007), l'âge (p=0,03), un triceps et un nerf suprascapulaire (NSS) déficitaires préopératoire (p=0,005). Conclusion : Le TSL procure une nette amélioration de la force et de la mobilité de manière fiable et reproductible. La force procurée par ce transfert atteignait en moyenne 70% du côté sain en isocinétisme. Ces résultats étaient nettement supérieurs lors des transferts isolés chez les patients jeunes.
|
Langue(s)
|
|
|
FM13
Clinical Evaluation of the Morbidity of Motor Nerve Transfer from the Radial Nerve to the Axillary Nerve.
Emmanuelle Richard, Lausanne FR
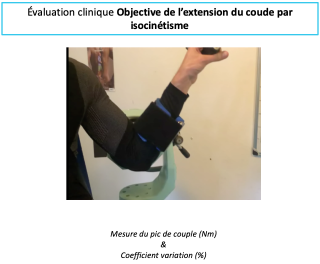
AbstractIntroduction : La morbidité du transfert de la longue portion du triceps (LPT) sur le nerf axillaire (NA) selon Somasak Leechavengvongs (TSL) est rapportée comme négligeable mais n'est pas l'objet de mesure objective dans la littérature. Nous en avons évalué la morbidité sur la force par un protocole standardisé et reproductible. Matériel et Méthodes : Par cette étude rétrospective monocentrique, 38 patients opérés d'un TSL entre 2008 et 2020 avec un triceps BMRC M5 préopératoire étaient éligibles. La force en extension du coude était évaluée par questionnaire, test BMRC, et isocinétisme de 90 à 0° en concentrique à 60 - 180°/s et en excentrique à 30°/s. Résultats : Vingt patients d'âge moyen de 25 ans (15 - 48) étaient volontaires pour une évaluation. Le recul était de 58 mois (6 -174). L’amyotrophie était visible pour 15/20 patients (75%), 7/20 (35%) avaient des contractures sur le triceps, et 12/20 (60%) une fatigabilité à l'exercice. Neuf triceps étaient M4 (11%) et 11 M5 (55%) au BMRC. La force en concentrique à 60, 180°/s et en excentrique à 30°/s était diminuée (respectivement -16,9 Nm, -14,8 Nm, et -16,3 Nm, p<0,001) soit -24%, -23% et -23% du membre sain. Les mesures objectives et subjectives étaient discordantes. Conclusion : La morbidité du TSL sur la force en extension du triceps se traduit par une diminution de force à M4 pour 11% des patients et -23% de force moyenne par rapport au côté sain en isocinétisme de manière homogène sur les différentes capacités du muscle. Cette morbidité, bien que non négligeable, ne semble pas avoir de conséquences à l’évaluation subjective. 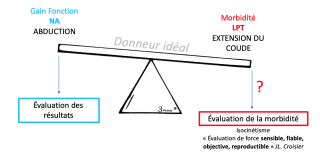
|
Langue(s)
|
|
|
FM14
Nerve transfer of teres minor motor branch to long head of triceps in C6–T1 brachial plexus palsy
Romain Baillot, Lausanne
AbstractIntroduction: Method: Results: Conclusions: 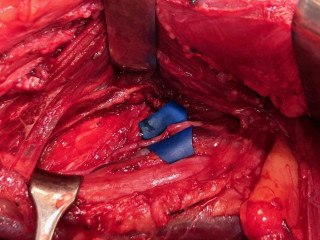
|
Langue(s)
|
|
|
FM15
Limitations of the Distal AIN-to-Ulnar Motor Branch Nerve Transfer for Pinch Recovery: A Case Series
Sören Könneker, Zürich DE
AbstractBackground: Methods: Results: Discussion: Conclusion: |
Langue(s)
|
|
|
FM16
Recurrent PIN Palsy Following Neuralgic Amyotrophy Treated with Decompression and Nerve Transfer
Sören Könneker, Zürich DE
AbstractBackground: Case Presentation: One year later, following a flu-like illness, the patient developed progressive recurrence of thumb extension and abduction weakness, leading to complete paralysis within 6 months. Hand therapy failed. Sonography suggested possible compression, prompting surgical re-exploration. Intraoperatively, an hourglass deformity of the PIN distal to the supinator canal was identified. Given the nerve’s poor appearance and uncertain prognosis, a distal nerve transfer was performed: the distal anterior interosseous nerve (AIN) was coapted to the distal PIN through a dorsal approach via membrana interossea dissection, selectively reinnervating APL, EPB, and EPL. Results: Conclusion: 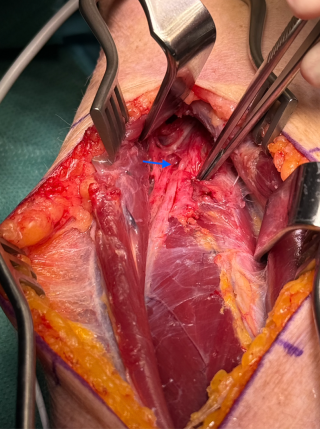
|
Langue(s)
|
|
|
FM17
Outcomes of traumatic brachial plexus injury in patients >50 years
Elalim Zen Vukovic, Bern
AbstractIntroduction Brachial plexus injuries (BPI) are associated with severe functional impairments of the affected limb, despite the availability of different treatment options. The incidence of these injuries is increasing among elderly individuals, likely due to a more active aging population; however, the underlying biology often remains unforgiving. The objective of this study was to assess which treatment strategies are most appropriate for patients aged >50 years with traumatic BPI. Materials and Methods In this retrospective analysis we evaluated patient data extracted from the electronical clinical records. We included consecutive patients with a traumatic BPI, aged >50 years, that were treated at our institution either operatively or conservatively. All cases exist in the period from September 2007 to January 2024. Patients with BPI other than trauma and < 50 years were excluded. Results The study included 10 patients, of which 9 were males. with a median age at time of injury of 63 (range 52-76 years). In 8 cases the BPI was due to polytrauma. This included 3 motorbike accidents, 2 ski injuries, 1 bike accident, 1 car accident and 1 non specified polytrauma. The remaining 2 cases were isolated traumatic BPI due to either fall or bike injury. C5-C6 segments were involved in 6 cases, 2 of which also affecting C7, 1 patient had distal BPI (C7-Th1), 3 patients a complete BPI. The right side was affected in 60% cases. Operative treatment was performed in 9 cases, median time from injury to first surgery 31.4 weeks (range 17-42.4). Of the 9 cases, 6 nerve transfers, 2 nerve reconstructions and one neurolysis were performed. Seven of these patients underwent a 2nd operation with a muscle transfer in 5 cases, neurolysis in 1 case and implantation of a pain electrode in 1 case. Two patients underwent a third surgery - 1 tendon transfer and 1 implantation of pain electrode. 50% patients suffered from persistent pain at last follow up. Only one patient benefited from the chosen surgical treatment. Nevertheless, 70% patients were satisfied and perform daily life activities with aids and trick movements to overcome the BPI consequences. Discussion Traumatic BPI in the elderly population is a challenging condition and the available operative options may not be of benefit for these patients. Despite the rather moderate results, an individual decision for surgery according to the needs and not just the age should be evaluated. |
Langue(s)
|
|
|
FM18
Key pinch restoration after high ulnar nerve injuries using Bertelli nerve transfer: A case series
Camilla Bo, Aarau
AbstractIntroduction High ulnar nerve injury commonly leads to severe intrinsic hand muscle weakness and sensory deficits in the ulnar digits. In 2018, Bertelli described a novel nerve transfer technique utilizing the motor branch of the opponens pollicis (OPB) to reinnervate the terminal division of the deep branch of the ulnar nerve (TDDBUN) with the goal of restoring key pinch. In this case series we report our preliminary experience with this technique in four patients who presented with intrinsic denervation following high ulnar nerve injury. Methods Four patients with confirmed proximal ulnar nerve injury were treated in our center, three of them were due to iatrogenic nerve injury following upper extremity surgery. Diagnosis was made by nerve imaging, electroneuromyography, and clinical examination, demonstrating loss of intrinsic function with a positive Froment sign and claw hand deformity. All patients underwent nerve transfer surgery in which, among others, the OPB motor branch was connected to the TDDBUN in the first commissure. Mean postoperative follow-up for all patients was 6 (2-12) months. Results Three patients were operated in 2024 and one in early 2025. Follow-up evaluations for the first patients demonstrated early functional recovery, with increasing function of the 1st interosseus and adductor pollicis muscles. Key pinch strength reached 47% (44-50) compared to the contralateral side in 3 patients at a mean follow up of 8 (3-12) months. The fourth patient was recently seen for her first follow-up 6 weeks after surgery and did not yet show measurable improvement. Notably, all patients reported subjective improvement in pain symptoms. Thumb opposition was strong and reached Kappandji 10 in all patients. Conclusion While longer follow-up and larger case series are required to draw definitive conclusions, our initial findings support the efficacy of the OPB-to-TDDBUN nerve transfer to restore key pinch function following high ulnar nerve injuries without significant donor morbidity. |
Langue(s)
|
|
|
FM19
Nerve Transfers for Radial Nerve Palsy: Clinical Results from a Prospective Case Series
Zeena Gerster-Barzanji, Zurich
AbstractBackground: Methods: Results: Conclusion: 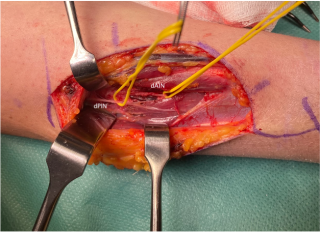
|
Langue(s)
|
|
|
FM20
Silvia Schibli, Nottwil
AbstractIntroduction Spasticity has been shown to negatively influence quality of life by restricting arm function, hindering self-care, causing pain, pressure sores and arthrosis. Personal care is often difficult, time-consuming, painful and place a significant burden on caregivers. Surgical interventions on the spastic upper limb aim to provide lasting correction of the deformities, thereby improving functional ability and facilitating activities of daily life such as hygiene and dressing. The aim of this study was to evaluate the impact of upper limb spasticity-correcting surgery using a comprehensive mixed-methods approach to gain deeper insights into the personal experiences of both patients and caregivers. Methods Qualitative semi-structured interviews were conducted 2.8 years (range 1-6 years) after surgery with nine caregivers and six patients. In addition, quantitative data were collected preoperatively and at 6 and 12 months postoperatively. This included the Arm Activity Measure (ARMA) score, resting limb posture, active and passive range of motion (AROM and PROM) of shoulder, elbow, wrist, fingers, and the thumb, as well as the House Functional Classification, which assesses the level of functional use of the upper extremity. Results The ARMA score improved from 12 preoperatively to 4.8 at 12-months follow-up, while hand function assessed by House score increased from 0.8 (does not use) to 2.4 (faire passive assist). The resting posture improved across all assessed joints with elbow position improving from 110° to 43° flexion and wrist position from 47° flexion to 12° extension. Qualitative data analysis corroborated these findings: both patients and caregivers reported easier personal care and dressing due to the improved limb position, as well as enhanced psychological well-being and satisfaction with the arm’s appearance: the more natural and relaxed appearance of the limb helped patients feel more confident and accepted in social interactions. Conclusion All participants, both patients and caregivers, experienced improvements in their everyday lives after spasticity-correcting surgery. The improved posture not only influences function but also psychological factors, leading to improved quality of life. |
Langue(s)
|
|
|
14:15 – 15:30
Saal B
|
Key Note LecturesCMC, PIP and AI - Spanish Insights
Sabrina Koch-Borner, Nottwil; Tamara Hauri, Bern
|
|
|
Sessions SSRM
|
||
Can We Stop the Progression of Incipient TMC Osteoarthritis? A Proprioceptive Protocol to Treat Early Rhizarthrosis.
Albert Domínguez Arasa, ES
|
Langue(s)
|
|
Collagen Behaviour on PIPJ Stiffness. Detection, Classification and Treatment Organization. Based on Clinical and Scientific Research
Vicenç Punsola Izard, ES
|
Langue(s)
|
|
Hand Therapy Meets AI: Are We Ready to Ride the Wave? Exploring the Present and Future of Artificial Intelligence in Clinical Practice, Patient Education, and Rehabilitation Pathways
Miguel Sánchez Guerra, ES
|
Langue(s)
|
|
Discussion |
Langue(s)
|
|
|
14:15 – 15:30
Saal E
|
Session Chirurgiens de la main en pratique privée
Frederik Hahn, Zürich; Sebastian Kluge, Zürich
|
|
|
Sessions SSCM
|
Traduction(s)
|
|
|
14:30 – 15:15
Saal A
|
Session principale IIArtificial Intelligence and New Technologies in Hand Surgery and Rehabilitation
Susanna Pagella, Lugano; Olga Politikou, Zürich; Mauro Maniglio, Zürich; Marco Keller, Schlieren
|
|
|
Joint Sessions SSCM / SSRM
|
||
AI in Hand Surgery- Ideas for Implementation
Daniel Herren, Zürich
|
Langue(s)
|
|
Detection and Treatment of Musculoskeletal Hand and Wrist Disorders with AI
Marco Keller, Schlieren
|
Langue(s)
|
|
Virtual Reality in Upper Limb Rehabilitation: A New Frontier in Therapy
Francesca Ferrario, Lugano; Susanna Pagella, Lugano
|
Langue(s)
|
|
Augmenting Clinical Reasoning in Hand Therapy: How AI Can Support Evidence-Based Practice
Bernadette Tobler, Bern
|
Langue(s)
|
|
Healthcare: Balancing Innovation with Security Risks
Francesco Costa, Zürich
|
Langue(s)
|
|
Discussion |
||
|
15:15 – 15:30
Saal A
|
Research Challenge – Design a Study
Miriam Marks, Zürich
|
|
|
Golden Hand Award-Sessions
|
||
|
15:30 – 16:00
|
Pause café |
|
|
Break
|
||
|
16:00 – 17:15
Saal B
|
Communications libres III
Isabelle Frank-Ziem, Zürich; Christa Jenni, Aarberg
|
|
|
Sessions SSRM
|
||
|
FM72
Hormone & Ergotherapie – Können wir über Hormone unser Tun evident erklären?
Barbara Aegler, Zürich
AbstractIntroduction : Méthodologie : Résultats : Implication pour la pratique : Littérature : |
Langue(s)
|
|
|
FM71
Application des principes psychologiques issus de l’économie à la thérapie de la main
Giovanni Leone, Zürich
AbstractHintergrund: Implikationen für die Praxis: Schlussfolgerungen: Disclosure: Dieses Abstract wurde in Kommunikation mit KI (ChatGPT) erstellt. |
Langue(s)
|
|
|
FM70
Driven by Hormones: The Science Behind Meaningful Activities - a Scoping Review.
Céline Delmée, Zürich
AbstractObjective: This scoping review explores literature on purposeful activities regulating stress in healthy adults, focusing on cortisol, oxytocin, perceived stress, and shared characteristics across them. Introduction: Purposeful activities are structured, goal-directed actions (Pierce, 2001), that may help regulate stress. Chronic stress negatively affects health and the healing of structures, emphasizing the need for evidence-based interventions (Hogan et al., 2023). While occupational therapy highlights meaningful occupations, purposeful activities may serve as effective intermediaries (Pierce, 2001). Hormonal markers such as cortisol and oxytocin offer objective physiological indicators for assessing stress (Pruessner & Ali, 2015). Methods: Included were studies on healthy adults engaging in purposeful activities, measuring at least one physiological (cortisol/oxytocin) and one psychosocial (perceived stress) outcome, published in English or German between 2012-2024. A comprehensive search was conducted in MEDLINE Complete, CINAHL Complete, and APA PsychInfo. Selection, extraction, and analysis followed Joanna Briggs Institute guidelines. Results: Fourteen studies were reviewed, covering activities such as singing, walking, social interaction, mindfulness, nature exposure and relaxation. These showed potential for stress regulation via effects on physiological markers and/or perceived stress. Shared characteristics included solo vs. group activity, sensory input, movement, nature connection, mindfulness and mood influence. Conclusions: Purposeful activities appear to support stress regulation by influencing hormonal and psychosocial responses. A better understanding of hormonal mechanisms can guide therapists and researchers in designing tailored interventions to promote health. More research is needed across diverse cultural contexts as well as the possible influence of gender.
Hogan, L.-M., Björklund Carlstedt, A., & Wagman, P. (2023). Occupational therapy and stress-related exhaustion – a scoping review. Scandinavian Journal of Occupational Therapy, 1–17. https://doi.org/10.1080/11038128.2023.2207802 Pierce, D. (2001). Untangling Occupation and Activity. The American Journal of Occupational Therapy, 55(2), 138–146. https://doi.org/10.5014/ajot.55.2.138 Pruessner, J. C., & Ali, N. (2015). Neuroendocrine Mechanisms of Stress Regulation in Humans. In Neuroendocrinology of Stress (pp. 121–142). John Wiley & Sons, Ltd. https://doi.org/10.1002/9781118921692.ch6
|
Langue(s)
|
|
|
FM74
Training the bounce factor
Chantal Wildhaber-Phillips, Zürich
AbstractLong-term negative stress can lead to health issues, such as cardiac disease, lowered immune function, depression and musculoskeletal disorders (MSDs) (Hoe et al., 2018). In Switzerland the prevalence of MSDs is high and is expected to rise (Engel et al., 2017). As more individuals seek to manage the stressors of daily life, the need for accessible, effective interventions grows. Resilience is the ability to overcome, adapt to or cope with stressful or disruptive life events (Turner et al., 2022). Occupational therapists (OTs), who specialise in promoting health and well-being through occupational participation are well positioned to support their clients in hand therapy to develop skills to manage stress and promote resilience (Matuska, 2014). The Mini-Activity-Approach (MAA) is an activity-based protocol for building resilience in everyday life (Aegler et al., 2019). Its popularity is increasing among OTs in Switzerland, Austria, the Netherlands, and Germany. In response to growing interest and feedback, the MAA development team initiated a revision process. In 2024, a small-scale exploratory study was conducted to gather expert perspectives for further development. The revision process is ongoing, and the current stage and direction of development will be presented. Our objective is to highlight the potential of occupational therapy to contribute meaningfully to preventive health care by supporting clients in the development of resilient, health-promoting habits. Aegler, B., Heigl, F., & Zischek, F. (2019). Das tut gut–Mini-AktivitätenAnsatz. ergopraxis, 12(09), 16-20. Engel, S., Bräm, R., Langenegger, T., Oesch, P., Stoll, T. (2017). Nationale Strategie Muskuloskelettale Erkrankungen (2017-2022). Rheumaliga Schweiz Hoe, V. C., Urquhart, D. M., Kelsall, H. L., Zamri, E. N., & Sim, M. R. (2018). Ergonomic interventions for preventing work‐related musculoskeletal disorders of the upper limb and neck among office workers. Cochrane Database of Systematic Reviews, (10). Matuska, K. (Ed.). (2014). The art and science of resilience. OTJR: Occupation, Participation and Health, 34(1), 2-3. Turner, J., Miller, W. C., Reid, H., Moecke, D. M. P., Crosbie, S., Kamurasi, I., Girt, M., Petlitsyna, P., Friesen, M., Towle, J., Knox, A., Winter, A., & Camp, P. (2022) How is resilience conceptualized and operationalized in occupational science and occupational therapy literature? Protocol for a scoping review. Cadernos Brasileiros de Terapia Ocupacional, 30, e3105-e3105. |
Langue(s)
|
|
|
FM63
Thérapie de la main chez le grand brûlé âgé : illustration par un cas clinique
Sarah Huber, Sion
AbstractIntroduction La rééducation fonctionnelle de la main brûlée est un enjeu majeur pour préserver l’autonomie. Chez les patients âgés, la fragilité tissulaire et les risques de complications cicatricielles justifient une prise en charge précoce, intensive et interdisciplinaire. Notre objectif est d’illustrer une stratégie de rééducation visant à restaurer la mobilité fonctionnelle du membre supérieur après brûlures sévères. Cas clinique Monsieur Y, 74 ans, présente des brûlures thermiques profondes (2ᵉ degré profond) sur 20 % de la surface corporelle, incluant le visage, le crâne, le cou, la partie supérieure du dos et la face dorsale et palmaire des deux mains, suite à une explosion. Après deux mois et demie en soins intensifs et plusieurs greffes cutanées, il est admis en rééducation. À l’admission, il présente des œdèmes des mains et des raideurs articulaires limitant la mobilité des doigts et des poignets, associées à des douleurs diffuses, un prurit important et un léger déficit sensoriel. Prise en charge Un programme spécifique est mis en œuvre, combinant :
Résultats À l’issue du séjour, le patient a retrouvé une autonomie complète dans les activités quotidiennes. On observe une récupération significative des amplitudes articulaires des poignets et des doigts, ainsi qu’une meilleure tolérance cutanée. Conclusion La rééducation de la main chez le grand brûlé âgé repose sur une approche globale, individualisée et coordonnée, visant à prévenir les limitations fonctionnelles et à optimiser la qualité de vie. Références Dewey, W. S., Richard, R. L. & Parry, I. S. (2011). Positioning, Splinting, and Contracture Management. Physical Medicine And Rehabilitation Clinics Of North America, 22(2), 229–247. https://doi.org/10.1016/j.pmr.2011.02.001 Kara, S. (2023). Effectiveness of early rehabilitation in hand burns. Turkish Journal Of Trauma And Emergency Surgery. https://doi.org/10.14744/tjtes.2023.22780 Young, A. W., Dewey, W. S. & King, B. T. (2018). Rehabilitation of Burn Injuries. Physical Medicine And Rehabilitation Clinics Of North America, 30(1), 111–132. https://doi.org/10.1016/j.pmr.2018.08.004 |
Langue(s)
|
|
|
FM64
Beurteilung und Behandlung von Verbrennungsnarben an der Hand
Fabienne Bor, Zürich
AbstractIntroduction : Objectif : Mesures : Le traitement préventif contre des contractures éventuelles est essentiel afin d’influencer positivement la formation cicatricielle. La pose précoce d'attelles fait partie intégrante du concept thérapeutique. Le degré de maturité et la stabilité des cicatrices dues à une brûlure peuvent être évalués à l’aide de critères tels que la couleur, la texture, l’élasticité et la fonctionnalité. Des tests et des instruments de mesure sont présentés afin de fournir une évaluation aussi objective que possible. Prochaines étapes : |
Langue(s)
|
|
|
16:00 – 17:15
Saal C
|
Communications libres IIISaddle Joint
Martina Greminger, St. Gallen; Nicolas Balagué, Sierre
|
|
|
Sessions SSCM
|
||
|
FM21
What Can Patients Expect After Thumb CMC Arthroplasty? Personalized Predictions for Pain and Function
Michael Oyewale, Zürich
AbstractAim: To develop and validate two machine learning models for predicting pain and hand function one year after thumb carpometacarpal (CMC) joint implant arthroplasty. Methods: We analyzed data from 377 patients who received a Touch® prosthesis (KeriMedical, Switzerland) between 2018 and 2024 and were prospectively documented in a clinical registry. Two models predicted pain during daily activities (Numeric Rating Scale [NRS], 0-10) and hand function (brief Michigan Hand Questionnaire [MHQ], 0-100) one year postoperatively. Extreme gradient boosting (XGBoost) was used with 23 clinical, radiographic, and patient-reported baseline variables. Models were trained with repeated cross-validation, tested on a held-out set, and evaluated using mean absolute error (MAE) and root mean squared error (RMSE). To quantify individual uncertainty, 80% prediction intervals (PI) were computed. SHAP (SHapley Additive exPlanations) values identified key predictors and their directional influence on outcomes. A dashboard was developed to visualize individual predictions along with prediction intervals and bootstrapped distributions. Results: The pain model achieved a bootstrapped MAE of 1.49 (95% CI: 1.45-1.54) and RMSE 2.24 (95% CI: 2.15-2.32), with predictions typically within 1.5-2 points of observed pain scores on the 0-10 NRS. SHAP analysis showed that better baseline health (EQ-5D-5L and EQ-5D-VAS), greater belief in treatment success, younger age, stronger grip strength, and lower baseline pain levels predicted lower residual pain. The function model reached a bootstrapped MAE of 12.44 (95% CI: 12.13–12.77) and RMSE of 17.27 (95% CI: 16.62–17.98). Patients with better baseline function (higher brief MHQ scores), stronger grip, better health (EQ-5D-5L), more thumb mobility, greater surgeon experience, and younger age were more likely to regain better hand function. Conclusion: We present interpretable machine learning models for individualized one-year outcome predictions after thumb CMC arthroplasty, including predictive uncertainty (Figure 1). These tools may support more realistic counseling and shared decision-making. Funding: None Conflicts of interest: Daniel B. Herren and Stephan Schindele have speaker contracts with KeriMedical. Other studies conducted at our clinic are funded by KeriMedical. 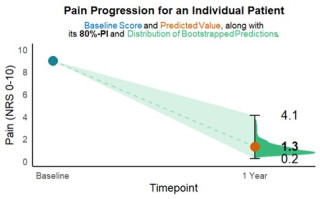
|
Langue(s)
|
|
|
FM22
Thumb CMC implant arthroplasty: Higher quality of life and lower costs than resection arthroplasty
Miriam Marks, Zürich
AbstractAim: The aim was to perform a cost-utility analysis comparing thumb carpometacarpal (CMC) implant arthroplasty with resection-suspension-interposition arthroplasty (RSIA) during one year after surgery. We hypothesized that thumb CMC implant arthroplasty would be more cost-effective than RSIA, with an ICER below the Swiss threshold of CHF 100,000 per quality-adjusted life year (QALY). Methods: In this prospective clinical trial, 80 working patients with thumb CMC osteoarthritis who underwent implant arthroplasty (Touch®) were included. Data were compared to 39 working patients from a previous study who received RSIA. Quality of life (EQ-5D-5L questionnaire), direct medical costs and productivity loss were measured for up to one year after surgery. The ICER was calculated to assess the costs per QALY. Sensitivity analyses were conducted for a 5-year extrapolation, including the higher risk of revision surgery for implant patients and outcomes for non-working patients. Results: One year after surgery, the implant group had a significantly higher quality of life (0.89 vs. 0.85 QALYs) and lower total costs (CHF 24'372 vs. CHF 30'866) compared to RSIA. Despite CHF 2'397 higher medical costs, implant arthroplasty was associated with CHF 8'892 lower productivity costs (Figure 1). The resulting negative ICER indicates implant arthroplasty is more cost-effective, with ≥99% probability of being cost-effective, even accounting for higher revision risks and non-working patients. Conclusion: Implant arthroplasty results in higher quality of life and lower overall costs than RSIA over one year. Despite higher direct medical costs, it is more cost-effective due to faster return to work and reduced productivity loss. Sensitivity analyses confirmed implant arthroplasty’s cost-effectiveness over five years, even with higher revision risks and a larger proportion of non-working patients. 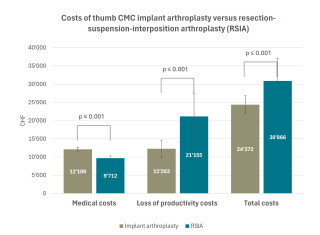
|
Langue(s)
|
|
|
FM23
At least 33 cases are required to flatten the learning curve in thumb CMC implant arthroplasty
Vanessa Reischenböck, Zürich
AbstractAim: The aim of this study was to (1) determine the learning curve for thumb carpometacarpal (CMC) implant arthroplasty and estimate the number of cases required for proficiency; (2) assess whether surgical experience influences the number of cases required to reach proficiency and (3) compare 2-year outcomes and revision rates between patients treated before and after the learning curve plateau. Methods: Data of 338 patients who received a Touch® prosthesis (KeriMedical) and who were prospectively documented in a registry were used. We included all operations performed by two highly experienced hand surgeons (A, B) and one less experienced specialist (C). The primary outcome measure was the number of surgeries required to achieve surgical proficiency, using the cumulative sum (CUSUM) method. In this method, surgery time and intraoperative radiographic exposure time are used as proxies for calculating the learning curve. Results: Surgery and intraoperative radiographic exposure times decreased for all surgeons as the number of cases increased. The resulting learning curve showed that surgical proficiency was achieved at case 33 for surgeon A and B, and case 40 for surgeon C (Figure 1). Mean surgery times were 39±8min, 43±7min and 59±19 min, respectively, and radiographic exposure times were 25±19s, 57±25s and 97±46s. Two-year outcomes and revision rates were not worse for patients who underwent surgery before achieving proficiency. The most frequent reason for revision was cup loosening. This stems from various factors beyond the technical learning curve. With increasing experience, broader indications led to selecting more challenging cases with bone deficiency and difficult soft tissue conditions. This increases the risk of intraoperative complications and less favourable postoperative outcomes. Conclusion: Our findings indicate a considerable learning curve for TMJ implant arthroplasty, with experienced surgeons achieving proficiency more quickly. Although outcomes before reaching the learning curve did not differ from those operated on later, we recommend comprehensive training when introducing this procedure and a high case volume to improve surgical skills. 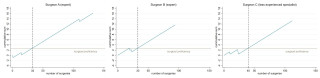
|
Langue(s)
|
|
|
FM24
Thumb CMC implant arthroplasty: A safe and effective treatment for patients aged 80 and older
Vanessa Reischenböck, Zürich
AbstractAim: The safety and efficacy of thumb carpometacarpal (CMC) implant arthroplasty in older patients remains uncertain, particularly due to the potential impact of osteoporosis on implant integration. The aim of this study was to investigate whether outcomes at one year post-surgery are comparable in patients over 80 years of age compared to those aged 60–70 years. Methods: This prospective registry-based study included patients who underwent thumb CMC implant arthroplasty (Touch®, KeriMedical, Switzerland). The one-year outcomes of patients aged ≥80 years (older group) were compared to those of patients aged 60–70 years (younger group). The primary outcome was pain during daily activities, measured on a 0–10 Numeric Rating Scale. Secondary outcomes included the brief Michigan Hand Outcomes Questionnaire (brief MHQ, 0–100), key pinch strength, and complications. Differences between the two groups were analyzed using the Mann-Whitney U test. Results: Eighteen patients aged 80–86 years and 175 patients aged 60–70 years were included. Preoperative pain scores were 6.9 (SD 2.1) for older and 7.1 (SD 1.8) for younger patients (p=0.88). At one year, pain decreased significantly to 1.3 (SD 1.8) in the older and 1.5 (SD 1.8) in the younger group, with no significant difference between the two groups (p=0.46, Figure 1). One-year brief MHQ scores were 80 (SD 20) for older patients and 86 (SD 17) for younger patients (p=0.27). Key pinch strength was 6.3kg (SD 2.2) in older and 6.7kg (SD 1.9) in younger patients (p=0.37). Intra- and postoperative complications such as trapezium fractures or implant loosening were absent in patients over 80 years. Conclusion: No significant differences in pain, hand function, or key pinch strength were found between patients aged ≥80 and 60–70 years at one year, with no complications in the older group. Although the sample size was small, the results suggest that thumb CMC implant arthroplasty is a safe and effective treatment for patients over 80 years when surgical indications are met. 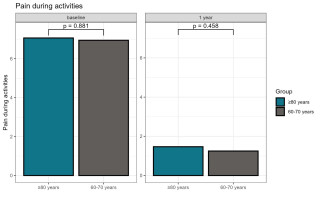
|
Langue(s)
|
|
|
FM25
Comparison of Rehabilitation Time, Costs, and Sick Leave between CMC I Prosthesis and Trapeziectomy
Claudio Hebeisen, Rheinfelden
AbstractIntroduction / Purpose of the Study
Materials and Methods
Results
Discussion and Conclusion
Clinical Relevance |
Langue(s)
|
|
|
FM26
Scaphometacarpal impingement after trapeziectomy: is fusion the solution?
Armin Pallaver, Luzern
AbstractIntroduction Scaphometacarpal impingement is one of the reasons for unsatisfying results after trapeziectomy. However, it remains unclear, why thumb subsidence after trapeziectomy occurs in some cases. A recent study recommended tendon-interposition and -suspension arthroplasty for revision in this situation, risking again instability and impingement. Other surgical options include implant arthroplasty and arthrodesis. We suppose that achieving stability with fusion of the first metacarpal base to the second metacarpal may be favorable in some cases.
Methods Retrospective, multi-center case series of 8 cases undergoing fusion of the first to the second metacarpal since 2000. We reviewed surgical technique and follow-up with fusion or revision surgery. Patient satisfaction was rated as good, fair or poor according to the clinical records.
Results Stable bony fusion was achieved in 6 cases at 3 months follow-up. Two cases needed revision arthrodesis with stable bony fusion at final follow-up. Bone graft from iliac crest was used in all cases, while fixation included k-wires, (cannulated) screws, plates or a combination of those.
Conclusion Fusion of the base of the first to the second metacarpal bone should be considered in cases with failed revision suspension arthroplasty on either side or as initial revision surgery after failed trapeziectomy in patients with manual work. Temporary transfixation of the first to the second metacarpal shaft reduces the lever arm on the arthrodesis site, enhances stability and may promote fusion. |
Langue(s)
|
|
|
FM27
Distal interosseous membrane reconstruction to treat distal radioulnar joint instability; 4 cases
Emmanuel Piguet, Genève
AbstractIntroduction Chronic distal radioulnar joint (DRUJ) instability impairs wrist kinematics, leading to a highly disabling condition and degenerative lesions. Numerous reconstructive techniques have been described either intra-articular, extra-articular or both. Recent literature has focused attention on the distal interosseous membrane (DIOM) and its contribution to DRUJ stability in all forearm position in addition to the TFCC. Material and methods We operated four patients who had chronic post-traumatic DRUJ instability. Preoperative clinical evaluation confirmed the instability, associated with painful pronosupination and a grip strength weakness (48 to 60% compared to the contralateral side). Arthrogram excluded arthritis in the DRUJ and TFCC lesion. Results All patients were reviewed one year after the surgery. DRUJ instability was systematically resolved. All patients were painless during pronosupination. Grip strength improved from 85 to 90% relative to the contralateral side. There was no difference in flexion–extension and pronation. Supination was reduced by 10 to 20°. All patients were able to resume working in the same occupation at a mean time of 4 months. Postoperative axial CT scans confirmed joint congruence restoration in pronation and supination. Discussion Conclusion 
|
Langue(s)
|
|
|
FM28
Palmar locked fracture dislocation of the distal radioulnar joint with delayed initial presentation
Giuseppe Broccoli, Winterthur
AbstractIntroduction/Purpose of the study/Hypothesis A palmar dislocation of the distal radioulnar joint (DRUJ), which is also fractured and misaligned locked, is a rare injury that can be overlooked at initial presentation. Based on current literature and a personal case, this rare injury is highlighted.
Material and method This case report presents a 23-year-old man with a three-month-old, volar locked fracture dislocation of the DRUJ resulting from a fall down stairs, which was initially overlooked. A complex open reconstruction of the DRUJ was performed to restore the function of the injured forearm and wrist. Postoperatively, the patient was immobilized for several weeks using an upper arm cast and the patient received accompanying hand therapy.
Results The patient's follow-up examination 12 months postoperatively showed pain at rest with a score of 0 (VAS 0–10), pain with load with a score of 1 (VAS 0–10), a relative grip strength compared to the unaffected side of 98%, a relative range of motion of the wrist compared to the uninjured side of 71%, a DASH score of 10 points, a Mayo Modified Wrist Score of 80 points as well as a Krimmer Wrist Score of 80 points. No complications occurred, and the patient was able to return to his original job and his martial arts activities.
Discussion and conclusion, clinical relevance Persistent wrist movement limitations after trauma, even with a seemingly correct x-ray, may indicate a serious injury to the DRUJ. Careful planning of a complex reconstructive surgery and the necessary follow-up care should be undertaken to achieve a satisfactory outcome for patients with an initially overlooked DRUJ dislocation. |
Langue(s)
|
|
|
FM29
5 years of implanting Touch® CMC-I prosthesis - lessons learned
Carla Kellenberger, Luzern
AbstractThe operative treatment of thumb carpometacarpal osteoarthritis has recently undergone a paradigm shift due to excellent early results of CMC-I prosthesis. However, with limited long-term outcomes beyond 10 years and challenges faced by earlier implants generations, careful consideration of their indications remains essential. This study presents the experiences of a teaching hospital’s hand surgery team over the first 5 years of implanting Touch® type CMC-I prosthesis, focusing on challenges and complications as “lessons learned”.
In our clinic, all patients who received a CMC-I prosthesis from 2019 to 2025 were identified. 182 cases were reviewed, involving 134 women, 48 men (average age 62y, range: 40-80y). Indications inculuded rhizarthrosis stages 2 or 3. Procedures were mainly outpatient under axillary plexus anaesthesia. Surgical technique involved: dorsal access between EPL and EPB, dorsal capsule resection, circumferential release of the MC I base, removal of trapezial osteophytes and radiologically guided cup drilling. Most cases involved a conical cup and a 15° angled neck. Postoperative care included rigid splinting for a week, followed by standardised therapy with a Comfort Cool brace and mobilisation, and initiation of load-bearing after 6 weeks, if X-ray controls were unremarkable. Beyond strength and mobility measurements, perioperative and postoperative complications and challenges were recorded. The analysis focuses on "lessons learned" rather than classic CROMs.
Complications occurred in 25.2% (46/182) of the cases. Revision surgery was required in 9.3% (17 patients). Issues included trapezium fractures (3) and dislocations due to incorrect cup placement (5). 4 cases needed a repositioning, while 2 required conversion to RSI arthroplasty. Tendinitis was observed in 22 cases, degeneration of the STT joint in 6 and MCP joint in 3 cases, respectively. Other complications included heterotopic ossifications (3), implant failure including polyethylene fracture (1) and neuropathic pain (8). While most were managed conservatively, some required surgical revision such as a 1st extensor compartment release, MCP joint arthrodesis, reoperation or neurolysis.
Results from the first five years of implanting CMC-I prothesis align with existing literature. We highlight challenges and the surgeon’s progression to guide less experienced colleagues in anticipating and avoiding issues or complications. |
Langue(s)
|
|
|
16:00 – 17:00
Saal A
|
Table ronde politique
Max Winiger, Zürich
|
|
|
Sessions SSCM
|
||
|
Table ronde politique – débat d’experts
Yvonne Gilli, Wil; Max Winiger, Zürich; Hans Rudolf Briner, Zürich
Table ronde politique – débat d’experts
|
||
|
17:00 – 17:15
Saal A
|
Puzzle Game
Sabrina Koch-Borner, Nottwil
|
|
|
Golden Hand Award-Sessions
|
||
|
17:15 – 17:30
|
Kurze Pause/Wechselzeit ohne Verpflegung |
|
|
Break
|
||
|
17:30 – 19:00
Saal A
|
Assemblée générale |
|
|
Sessions SSCM
|
||
|
17:30 – 19:00
Saal B
|
Assemblée générale |
|
|
Sessions SSRM
|
||
|
20:00 – 20:15
|
Soirée de fête conjointe |
|
|
Break
|





