Anzeige
Wissenschaftliches Programm
|
Ab 07:30
|
Registrierung |
|
|
08:00 – 09:30
|
Strahlenschutz-Kurs |
|
|
Club Casino
SK
|
Philipp Honigmann, Bruderholz; Stephan Schindele, Zürich
|
|
Einführung zum Strahlenschutz
Philipp Honigmann, Bruderholz; Stephan Schindele, Zürich
|
|
|
Praktischer Strahlenschutz
Jacqueline Metzen, Kleingurmels
|
|
|
|
08:15 – 09:30
|
Gong Show |
|
|
Theatersaal
GS
|
Philipp Honigmann, Bruderholz; Thomas Mészáros, Fribourg; Stefanie Schmitt, Luzern
|
|
|
FM29
Intraoperative findings, treatment option and follow-up in an acute two-level skier’s thumb injury
Alina Strohmaier, Chur; Mathias Häfeli, Chur
DetailsIntroduction Skier`s thumb injuries are frequent sports injuries. Rarely, so-called two-level injuries have been described in the literature, where an osseous lesion and a Stener lesion without attachment of the ulnar collateral ligament (UCL) to the bone fragment occur simultaneously. We report a rare case of an acute two-level skier’s thumb injury, intraoperative findings, treatment with anatomic reduction and follow-up results. Material and methods A 46-year-old patient presented to our emergency department with pain of the right thumb after a skiing accident. Clinical examination revealed significant ulnar instability. The X-ray showed a dislocated and 90 degrees rotated avulsion fracture of the proximal phalanx base as well as a conspicuous saucer-type small ulnar-sided fragment at the level of the distal first metacarpal bone. In the ultrasound of the first metacarpophalangeal joint we saw an irregularity of the UCL and rupture of the adductor aponeurosis, which was suspicious for a Stener lesion. Because of these findings we indicated surgery. Intraoperatively the UCL was found flipped back at the ruptured aponeurosis with a small bone fragment attached. Incision of the aponeurosis and the capsule, revealed the dislocated and rotated fragment of the proximal phalanx. Refixation of the avulsion fragment and the distal ligament with one bone anchor was performed. The intraoperative X-ray showed an anatomical reduction. Results After 4 weeks of immobilization the fracture was mostly consolidated, the joint was stable and the patient pain free. After three months the patient had an equivalent range of motion in both thumbs. Discussion and conclusion Compared to other skier`s thumb injuries, here it was important to recognize the rotation of the big fracture fragment and to recognize the second smaller fragment in the X-ray. Also the case is a good example that even if ultrasound was not performed perfectly, it led to additional information - the suspicion of a Stener lesion. To recognize these deviations from other skier`s thumb injuries, was important to make the decision to perform surgery. The assumption that the big bone fragment presents the location of the distal part of the ulnar collateral ligament can lead to false treatment decisions. Particularly in frequent cases it`s important to stick to an established diagnostic algorithm, be alert of deviations from the typical injury and to be flexible in treatment options according to intraoperative findings. |
||
|
FM30
Schwannoma of the digital nerve – a rare finding
Carla Kellenberger, Chur; Mathias Häfeli, Chur; Christian Wirtz, Chur; Tim Cordier, Chur
DetailsIntroduction Soft-tissue tumors of the hand are common and most often benign. Rare entities should be considered as they can affect surgery and aftercare. We report of a schwannoma of the digital nerve as one reason for soft-tissue swelling in the finger. Material and Method A 46-year-old woman presented with a slowly growing mass over the last 3 months at the ulnopalmar side of her ring finger. The mass was painful and progressively compromising the flexion of the finger. There was neither an impairment of capillary refill or sensibility nor a Tinel sign. We palpated a firm, elastic mass, which was mobile to surrounding tissue. Ultrasound showed an 11x4x6mm well defined, rounded, hypoechoic mass in proximity to the ulnopalmar digital artery without any Doppler flow. The ulnopalmar digital nerve was not clearly identifiable. Result During Surgery, we identified the ulnopalmar neuro-vascular bundle. The tumor presented as an elliptic, beige mass, incorporated in the digital nerve's sheath and was bluntly separated from the nerve fascicles. Histologic results confirmed the diagnosis of a schwannoma. After 4 weeks, the patient was pain-free with a good range of motion. There was a painless Tinel sign over the digital nerve with normal sensibility. Discussion A schwannoma is a benign tumor growing from Schwann cells and with about 90% the most common peripheral nerve tumor (Pertea2022). Usually growing slowly and eccentrically in the peripheral nerve sheath it can remain asymptomatic until it causes functional deficit or pain. To define the relationship to adjacent structures diagnostic imaging is helpful. MRI can differ between a malignant and benign lesion but cannot distinguish a schwannoma from a neurofibroma. Ultrasound shows a well-defined, fusiform, hypoechoic mass with loss of fascicular patterns. Final diagnosis can only be made histologically. Only few cases of occurrence in the hand were reported so far. Still, it should be considered as a differential diagnosis of neoplasms such as ganglion cyst, giant cell tumor, lipoma or neurofibroma. If symptomatic, surgical excision is advised. |
|
|
|
FM31
Chronic Finger Joint Luxation; Having A Go With The “MiniFlo”
Andrej Cousin, Bern; Dominique Merky, Bern; Esther Vögelin, Bern; Nadja Grob, Bern
DetailsIntroduction: Chronic luxation of a finger joint, either the metacarpophalangeal (MCP) or proximal interphalangeal phalanx (PIP) joint, can be challenging to treat. After open reduction and arthrolysis, reluxation or impaired range of motion (ROM) are often observed. We think the key of success lies in postoperative immediate guided, controlled passive motion of the involved joint. With the use of the MiniFlo™ (Citieffe, Bologna, Italy), an external distraction device, successful management may be achieved. Method: We report two cases of chronic MCP V respectively PIP II joint luxation. In both cases, initial reduction through a dorsal and palmar (MCP) respectively palmar incision (PIP) was unsuccessful, with reluxation and impaired ROM after surgery. In a second attempt six months, respectively four months later, an arthrolysis and reposition of the chronically dislocated joints in combination with installation of the external fixateur MiniFlo, to start with immediate postoperative controlled passive motion for 4-8 weeks, was performed. Because of reluxation, pain and joint stiffness, the only alternative would have been an arthrodesis. Results: On average, a joint motion from 0° pre-operatively to about 90° ROM could be documented about two to three months after dismantling the MiniFlo. During the follow up time, eight to twelve months after the second surgery, no reluxation or subluxation in either case was observed and ROM could be maintained. So far, no “third” surgery for arthroplasty because of joint-pain was necessary. Conclusion: An early controlled, passive joint motion, managed with the “MiniFlo”, instead of a postoperative immobilization phase, is a promising therapy extension in chronic finger joint luxation. Especially if arthrodesis would be the only other option to treat rigid, painful, degenerative joint arthritis. Pre-requisite is a motivated and compliant patient. |
|
|
|
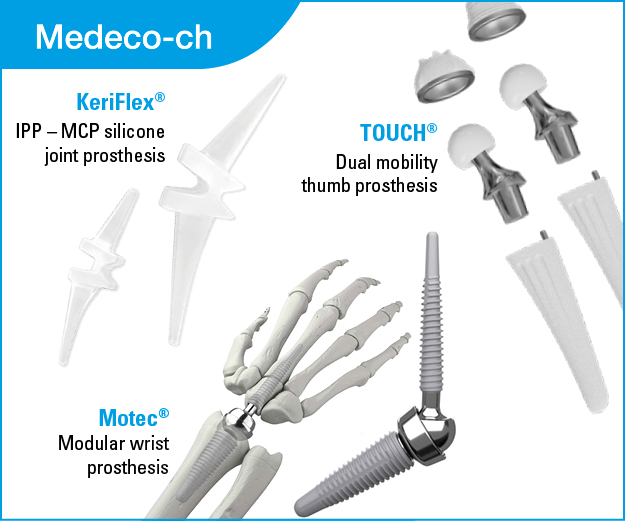
FM32
One year results and comparison of two double mobility prostheses for trapeziometacarpal arthritis
Eva Winand, Frauenfeld; Moritz Scholtes, Münsterlingen; Sebastian Hediger, Frauenfeld
DetailsObjective: To analyse our short term clinical and radiographic results for double mobility prostheses for trapeziometacarpal arthritis using two different implant systems and hence also focusing on possible differences between the two systems. Methods: Patients treated with a double mobility implant for trapeziometacarpal arthritis were prospectively included in a registry since February 2021. The implant type used was either MAÏA™, or TOUCH®, depended on the location where the operation was performed (our clinic performs operations equally at two locations). We recorded data preoperatively, at 6 weeks, 3 months and 1 year. Patient reported outcome was assessed using the bMHQ. Pain was rated at rest and during daily activities. Key pinch strength and thumb mobility using the Kapandji score was measured. In the radiographic assessment we focused on cup position (i.e. eccentricity – defined as the cup breaching or touching the cortex of the trapezium) and in the short term on signs of cup loosening. Further, we recorded complications and revisions. Results: Until submission of the abstract, we have 47 implants in our registry, of whom 25 were operated on 1 year ago or earlier and were therefore considered in this analysis. No revisions had to be performed so far, resulting in a survival rate of 100%. As the sole complication, we encountered one case of De Quervain’s tenosynovitis. This case was treated with additional surgery. At one year, 19 patients were available for follow-up (8 MAÏA™, 11 TOUCH®). Overall, the bMHQ score increased from mean 45.9 (CI: 42.2-49.5) preoperatively to 85 (CI: 82.4-89.4). Pain at rest/ during daily activities decreased from 8 (CI: 7.7-8.3)/ 8 (CI: 7.7-8.3) to 0.15 (CI: 0.01-0.29)/ 0.4 (CI: 0.2-1.11). Key pinch strength increased from 4.2kg (CI: 3.6-4.8) to 5kg (CI: 4.6-5.4). Thumb mobility showed a slight improvement. No significant difference in the respective results between the two implants could be detected. Radiological analysis showed no case of cup loosening until final follow up. Eccentric cup position occurred in four cases (equally allotted between the two implants) but without detectable implications on clinical outcome. Conclusions: Our results, despite a small patient number, using two double mobility implants for treating trapeziometacarpal arthritis are very promising and comparable to the current literature. No detectable difference in the clinical or radiological analysis between the two implants could be documented. |
|
|
|
FM33
To amputate or not? Extreme digital salvage after resection of a recurrent giant cell tumor
Crinu Baesu, Aarau; Jan Plock, Aarau; Florian Früh, Aarau
DetailsAbstract Giant cell tumors of tendon sheath (GCTTS), also known as pigmented villonodular tenosynovitis, are the second most common soft tissue tumors after ganglion cysts. They can be divided into masses with localized or diffuse growth pattern. We herein report a case of a GCTTS recurrence in a 54-year-old male patient.
The patient suffered from a left middle finger GCTTS recurrence. Radiographs and magnetic resonance (MR) imaging revealed involvement of the ulnar neurovascular bundle, the flexor and extensor tendons as well as a destruction of the distal interphalangeal (DIP) joint. The patient was an active sportsman and wished for digital preservation. Hence, radical excision with en-bloc resection of the DIP joint was performed, resulting in a sub-circumferential 4x3 cm defect. The joint was fused using a cannulated compression screw and the soft tissue defect was reconstructed with a retrograde-arterialized free venous flap from the ipsilateral forearm. One arterialized inflow vein and two outflow veins (1 dorsal and 1 palmar) were included in the flap. The further clinical course was uneventful with no radiographic or MR signs of recurrence at 6-months. Histopathology revealed a GCTTS without signs of malignant transformation. At 4 months after surgery, the patient was able to return to all previous recreational activities.
Recurrent and infiltrative GCTTS in fingers are a challenging clinical problem. In our case, the patient opted for digital preservation with microvascular tissue transfer. Free venous flaps are an excellent reconstructive option for extensive digital defects because they can be tailored to almost any defect geometry. Furthermore, depending on the forearm anatomy, they can also serve for concomitant digital nerve reconstruction using terminal branches of the lateral or medial antebrachial cutaneous nerves. However, amputation should always be discussed with patients suffering from massive GCTTS recurrence. Compared with potentially complicated microvascular reconstruction, digital amputation offers a faster treatment with a lower risk for long-term complications.
Taken together, massive distal digital defects associated with GCTTS recurrence are a reconstructive challenge. Free venous flaps are an excellent option for digital salvage in these cases. |
|
|
|
FM34
Disseminated Nocardia Paucivorans Infection with ulnocarpal lesions, pulmonary and CNS involvement
Peter Mohos, Bruderholz; Philipp Honigmann, Bruderholz; Georg Julian Claas, Bruderholz; Marco Keller, Zürich
DetailsIntroduction To our knowledge, no disseminated Nocardia infection, presenting with subcutaneous lesion as a single sign of this disseminated disease has been until now reported. During the clinical examination on the emergency department, there was no suspicion of either pulmonary or cerebral involvement. |
|
|
|
FM35
Exceptional Manifestation Of Synovial Chondromatosis In A Small Finger - A Case Report
Léonie Hüsler, Luzern; Alain Schiffmann, Luzern; Urs Hug, Luzern
DetailsIntroduction Synovial chondromatosis is a rare benign disorder. It is characterized by the metaplasia and proliferation of synovial tissue, resulting in the formation of loose cartilaginous or osteocartilaginous bodies within the synovial membrane of joints. It predominantly affects large joints, while its occurrence in small joints, such as finger joints, is uncommon. The malignant degeneration into chondrosarcoma has been described but is rare. The typical radiographic presentation of synovial chondromatosis is characterized by multiple calcified cartilaginous loose bodies. In advanced stages, it may progress to the formation of a giant solitary synovial chondromatosis through the fusion of the loose cartilaginous bodies. This case report presents an interesting case of synovial chondromatosis, highlighting the clinical manifestations with significant functional impairments and the successful treatment outcome.
Material & Methods A comprehensive work-up of the patient's medical records, including history, examination findings, radiographic imaging, and surgical intervention, was performed.
Results The case report describes a 40-year-old male cook who presented with a progressive swelling of the distal interphalangeal joint of the small finger, persisting for 15 years. The swelling was indolent but hindered the patient's ability to grip knives properly due to restricted mobility. The patient's inability to use the non-functional finger in daily activities led to a strong desire for amputation. Although joint disarticulation was considered as a therapeutic option, the patient ultimately underwent tumor resection, which included extensor and flexor tendon tenolysis. Remarkably, the patient achieved a full restoration of range of motion and became completely symptom-free.
Conclusion By presenting this exceptional case report, it serves as a reminder to hand surgeons about the potential involvement of smaller joints, such as the distal interphalangeal joint, in synovial chondromatosis. |
|
|
|
FM36
Die Sattelgelenksprothese als Therapieoption bei Metakarpale-I-Trümmerfrakturen
Stephanie Luz, St. Gallen; Jörg Hainich, St. Gallen; Johannes Fuchs, St. Gallen; Dominik Spühler, St. Gallen
DetailsEinleitung: Die Behandlung intraartikulärer Trümmerfrakturen der Metakarpale-I-Basis ist anspruchsvoll und zeigt nach konventioneller Frakturversorgung häufig unbefriedigende Ergebnisse bei nicht anatomisch wiederherstellbarer Gelenkfläche mit Ausbildung einer sekundären Arthrose. Im Bereich der elektiven Behandlung der Osteoarthritis des Daumensattelgelenks zeigt die CMC-1 Prothese zuverlässige, sehr gute mittel- und inzwischen auch langfristige Ergebnisse. Die Verwendung derselben als Frakturprothese bietet sich als Rückzugsmöglichkeit in komplexen Fällen an. Hierzu finden sich in der Literatur bis dato keine Fallberichte. Wir präsentieren den ersten Fall einer CMC-1-Prothesenimplantation bei intraartikulärer, dislozierter, mehrfragmentärer Metakarpale-I-Basisfraktur als alternative Frakturversorgung bei einer rüstigen, betagten Patientin. Ergebnisse: Im postoperativen follow up kann eine vollständige Schmerzfreiheit bei vollständig freier Beweglichkeit des linken Daumens mit Wiederherstellung der Selbständigkeit im Alltag erreicht werden. Zusammenfassung: Die primäre Implantation einer Daumensattelgelenksprothese bei nicht anatomisch rekonstruierbaren Trümmer- oder Defektfrakturen der Metakarpale-I-Basis ist eine technisch einfach umsetzbare Rückzugsmöglichkeit und kann als Alternative zur herkömmlichen Frakturversorgung dienen. Postoperativer Verlauf und Outcome unterscheiden sich nicht von der Implantation bei Rhizarthrose. Zur Evaluation der indizierten Frakturtypen, dem geeigneten Patientenalter sowie dem langfristigen Outcome ist eine randomisierte, prospektive Studie in unserem Haus geplant. |
|
|
|
FM37
Diagnostic accuracy of wrist MRI in comparison to wrist arthroscopy regarding TFCC lesions
Christian Spies, Langenthal; Frank Unglaub, Bad Rappenau (DE)
DetailsIntroduction: The purpose of this study was to arthroscopically verify MRI diagnostic accuracy for triangular fibrocartilage complex (TFCC) lesions in a regular clinical environment. Results: Diagnostic accuracy of MRI for TFCC lesions is poor in comparison to wrist arthroscopy as the reference standard. Technical specifications for MRI of the wrist are heterogeneous among the radiologists. These parameters have not improved accuracy of TFCC evaluation at large. Conclusion: The accuracy of MRI in a regular clinical environment still remains inferior to wrist arthroscopy for detection of TFCC lesions. Development of a standard MRI protocol may be implemented on a regular basis and application of the Palmer classification for TFCC lesion should be sought. |
|
|
|
FM38
High-intensity focused ultrasound therapy for an osteoidosteoma in a pediatric finger: a case report
Joëlle V. Hüppi, Winterthur; Christoph Andreas Binkert, Winterthur; Nadja Zechmann-Müller, Winterthur
DetailsIntroduction: High intensity focused ultrasound (HIFU) is a potential non-ionizing and non-invasive application for benign and malign disease. Ultrasonic waves are concentrated in a specific manner to achieve high level of energy in specific area of tissue. This leads to an increase of temperature and to necrosis due to coagulation resulting in irreversible damage of the tissue. We will describe one pediatric case where HIFU was successful in the treatment of an osteoidosteoma. Material and Methods: A seven-year-old boy presented in our department for hand surgery due to notable indolent swelling of the distal phalanx of the right ring finger. Neither recent trauma, nor any history of rheumatological disease in family history was memorable. Clinical examination showed significant enlargement of the distal phalanx with minimal pain on palpation and unlimited mobility. Conventional radiography showed discrete fuzzy sclerosis of the metaphyseal part of the growth plate. MRI was not conclusive, but suspicious for chronic osteomyelitis. Bone biopsy showed reactive change with no signs for acute inflammatory event. Periodic checks were performed, with no change in clinical and radiographic aspect. Nine months after the first appointment, the patient presented with pain after minor trauma and increase of the swelling. Radiography showed a visible light spot, so called nidus, in the distal phalanx leading to a suspected diagnosis of an osteoidosteoma. In a synopsis of the present findings, MRI-guided HIFU (MR-HIFU) was recommended. Results: One year after the first appointment, MR-HIFU was performed to destroy the nidus of the osteoidosteoma and to prevent further hypertrophic growth. Six months after the intervention the patient presented with no further exponential growth and the difference to the other phalanges was minimized. Furthermore, radiography showed no retention of the nidus with a plane distal phalanx. Discussion: MR-HIFU is a promising approach in the non-invasive treatment of tumorous neoplasm. Because of its non-ionizing ultrasonic waves, there is no upper limit in dosing. The deposition of heat is in general limited by the surrounding tissue, which should not be exposed to overheating. The main factors preventing MR-HIFU treatment are thick bone around the nidus, a superficial position with risk for skin burn and the vicinity to neural structures. Osteoidosteomas are generally rather small and therefore well suited for MR-HIFU. |
|
|
|
FM39
A case of destructive osteoarticular tuberculosis of the thumb interphalangeal (IP) joint
Xavier Beaud, Villars-sur-Glâne; Thomas Meszaros, Villars-sur-Glâne; Nina Fuchs, Villars-sur-Glâne
DetailsAbout a quarter of the world's population is latent infected with Mycobacterium tuberculosis. In Switzerland, the incidence remains very low, especially in the native population. Digital localization is uncommon, representing 4-8% of cases of osteoarticular tuberculosis. Method We report the case of a 49-year-old bricklayer of southwestern European origin, who showed a painful atraumatic swelling of the IP joint of his right thumb for several weeks, without improvement after an empirical antibiotic treatment and an incision for drainage of a suspicious panaritium. Synovial hypertrophy but no frank effusion was found sonographyically, an osteopenia and narrowing of the IP joint space on conventional radiographs. The appearance of a dorsal fistula about one month after the initial presentation raised the suspicion of chronic septic arthritis. A debridement with sampling for microbiological and histopathological analysis was performed. Conventional microbiological analysis revealed no bacterial growth, but the histopathology severe chronic granulomatous synovitis and partially necrotic osteomyelitis. The diagnosis of Mycobacterium tuberculosis osteoarthritis was confirmed by subsequent PCR analysis. Systemic evaluation revealed associated pulmonary tuberculosis, and antibiotic treatment was initiated. After an initial positive postoperative period, the IP joint remained symptomatic at three months, with localized pain, decreased range of motion, and progressive destruction on conventional radiograph. A second debridement with sampling was performed and the joint was fused with Kirschner wires. No bacterial growth, residual granulomatous inflammation, or giant cells were identified in the intraoperative samples. The local pain decreased rapidly. At the last follow-up before abstract submission (11 weeks), the arthrodesis was not completely healed, and immobilisation with a splint was continued. Conclusion Even if it remains very rare in developed countries, tuberculosis should be considered as a differential diagnosis in cases with atypical presentation of digital osteoarthritis. Although the literature on tuberculous interphalangeal osteoarthritis is sparse, its treatment appears to be primarily medicamentous. Surgery is initially needed as diagnostic tool and sometimes to treat symptomatic sequelae in the later course of the disease. As treatment for symptomatic destruction of the interphalangeal joint of the thumb, arthrodesis appears to be a valuable option. |
|
|
|
08:15 – 09:30
|
Speed Dating Session |
|
|
Ballsaal
SP
|
Julie Dziwornu, Aarberg; Lea Feller, Winterthur
|
|
|
09:30 – 10:00
|
Kaffeepause |
|
|
10:00 – 11:30
|
Freie Mitteilungen IVFinger joints & Miscellaneous |
|
|
Ballsaal
SGH-FM4
|
Moritz Scholtes, Münsterlingen; Lea Estermann, Zürich
|
|
|
FM40
Is PIP surface replacement recommended in patients with severe longitudinal joint axis deviation?
Xenia Startseva, Zürich; Daniel Herren, Zürich; Miriam Marks, Zürich; Stephan Schindele, Zürich
DetailsObjective: The aim was to compare the 2-year outcomes after proximal interphalangeal (PIP) joint surface replacement in joints with more than 15° preoperative deviation to the longitudinal finger axis versus joints without any preoperative deviation. Methods: Patients who received a primary single surface replacing PIP arthroplasty (CapFlex PIP, KLS Martin, Germany) were included. Longitudinal finger axis deviation at the PIP joint level was measured and classified as: no deviation (<5° deviation to the longitudinal finger axis), moderate deviation (5°-15°) or severe deviation (>15°). Active range of motion (ROM) of the PIP joint was measured. Patients completed the brief Michigan Hand Questionnaire (MHQ) and rated their pain during daily activities on a Numeric Rating Scale (0-10). Baseline and 2-year outcomes between patients with and without deviations were compared with the Mann-Whitney U test.
Results: Out of 216 fingers initially operated, there were 7 (3.2%) that required revision surgery. Four fingers had severe axis deviation before surgery and 3 were classified with moderate deviation. The reasons for revision were stiffness (n=4), suspected metal intolerance (n=1), late low-grade infection (n=1), and luxation of the implant components (n=1). Before surgery, 47 patients had a severe axis deviation and 39 had no deviation. At the 2-year follow-up, only 4 of the 47 patients still had a severe axis deviation; all remaining fingers could be corrected to a deviation of less than 15°. At 2 years, patients with severe and without deviation had a mean ROM of 63° (95% Confidence Interval [CI]: 58-68) and 59° (CI: 52-65) (p=0.4), respectively. In addition, the respective mean pain scores were 2.1 (CI: 1.4-2.8) and 1.7 (CI: 1.2-2.2) (p=0.8), and the brief MHQ scores were 72 (CI: 66-79) and 75 (CI: 71-80) (p=0.7). Conclusion: Clinical and patient-reported outcomes at 2 years were similar between patients with severe and without preoperative axis deviation, and the joint axis could be corrected in most cases. The incidence of PIP joint revision surgeries was higher with a preoperative longitudinal joint axis deviation, yet the reasons for revision cannot be directly related to this factor. Stiffness may be related to axis deviation, as these joints were immobilized longer after surgery than straight fingers. We recommend a surface replacing implant to correct severe axis deviations, but the risk of revision surgery needs to be considered. |
|
|
|
FM41
Complications after thumb CMC implant arthroplasty: Our 5-year experience
Daniel Herren, Zürich; Miriam Marks, Zürich; Stephan Schindele, Zürich
DetailsAim: The aim was to provide a comprehensive assessment of complications and revision surgeries up to 5 years after thumb carpometacarpal (CMC) dual-mobility implant arthroplasty. Methods: All patients with osteoarthritis of the thumb CMC joint who underwent primary implant arthroplasty (Touch®, KeriMedical) between June 2018 and April 2023 were prospectively documented in a registry and included in this analysis. Intra- and postoperative complications and its treatment strategies were documented. Clinical (key pinch, grip strength) and patient-reported outcomes (pain, brief Michigan Hand Outcomes Questionnaire) before surgery and at 2-year follow-up were compared between patients with and without complications using an independent t-test. Implant survival up to 5 years was estimated using the Kaplan-Meier method. Results: A total of 281 patients with a mean age of 64 (±9) years were included. Thirty-three complications (12%) occurred and 8 implants (2.8%) required revision, resulting in an estimated 5-year survival rate of 96% (95% confidence interval: 92%-98%). Reasons for revision were symptomatic implant loosening, dislocation, or migration. In 4 cases the components were changed and in the other 4 cases a resection arthroplasty was performed. The most frequent other complications were de Quervain tenosynovitis (n=12) and trigger thumb (n=6), which were treated with either steroid injections or soft tissue surgery. There were also 3 cases of intraoperative trapezium fractures that were successfully fixed with a suture cerclage. There were no differences in the 2-year outcomes between patients with and without complications (p>1). Conclusion: Thumb CMC dual-mobility implant arthroplasty shows high implant survival and soft-tissue complications can usually be resolved with an injection or minor surgery. The reasons for revision were mainly iatrogenic, i.e. implant placement was not optimal in our first cases or we tried to implant a prosthesis despite a small or insufficient trapezium. Therefore, we recommend good training of the surgeon and careful indication. |
|
|
|
FM42
Basal osteotomy of the first metacarpal using patient-specific guides – Clinical & 3D CT-based analysis
Cléa Nüesch, Zürich; Andreas Schweizer, Zürich; Lisa Reissner, Zürich
DetailsIntroduction Combined extending and ulnar adduction osteotomy using patient-specific guides and instrumentation showed good results in early-stage thumb arthritis. The aim was to investigate the subjective and clinical results of ten early to advanced stage trapeziometacarpal osteoarthritis and to compare the joint loading area before and after surgery. Method Between November 2020 and December 2021, we included nine patients with early to advanced trapeziometacarpal osteoarthritis in a prospective observational study who underwent Wilson extension osteotomy using preoperative 3D planning and patient-specific guides at our institution. Preoperative and one-year postoperative subjective assessment was based on a visual analogue scale (VAS) for pain and MHQ score. Range of motion (ROM) and grip strength data were investigated. Postoperative computed tomography with the corresponding 3D models was used for comparison with the preoperative plan. For the measurement of the minimum joint space between the trapezium and the first metacarpal bone, the bone-to-bone distance maps were calculated with the CASPA Result Pain and patient satisfaction improved significantly at the one-year follow-up. The mean ROM of the metacarpophalangeal and interphalangeal joints was similar to the preoperative ROM. The minimum joint space distance remained approximately unchanged from preoperative to postoperative, with a mean distance of 0.1 mm (SD 0.2 mm) preoperatively to 0.2 mm (SD 0.3 mm) postoperatively. The peak load zone of the trapezium articular surface shifted postoperatively by an average of 0.4 mm (SD 1.4 mm) (p=0.110) to radial and 0.1 mm (SD 1.2 mm) (p=0.515) to volar. Conclusion Extension and ulnar adduction osteotomy were found to result in satisfactory patient condition not only in Eaton stage I but also in II and III osteoarthritis, possibly leading to a change in the loading pattern of the joint surfaces. However, computed tomography-based three-dimensional analyses could not show a significant displacement of the peak load zone in dorsal-radial direction, as the values obtained are considered too small. Nevertheless, trends emerged suggesting that flatter pressure distribution and a dorsal displacement of the peak load zone could contribute to an improvement in pain and patient satisfaction.
|
|
|
|
FM43
Quantitative stiffness analysis of the proximal interphalangeal joint after joint replacement
Gabriella Fischer, Zürich; Lisa Reissner, Zürich; Maurizio Calcagni, Zürich; Raphael Surbeck, Zürich; Esin Rothenfluh, Zürich; William R. Taylor, Zürich
DetailsIntroduction One of the most challenging problems of hand surgery is the treatment (and prevention) of proximal interphalangeal (PIP) joint stiffness. At present, functional outcome measures are mostly based on range-of-motion in the finger joints. We propose a method for the quantitative assessment of PIP joint stiffness and applied it in patients after PIP joint replacement surgery. Methods Seven patients with a minimum follow-up period of 1 year since PIP implant arthroplasty (Swanson or CapFlex) in context of osteoarthritis (OA) were included. PIP joint stiffness of all long fingers in both hands was measured, using a newly developed finger stiffness measurement device (FSMD) and assigned to the following categories: healthy, Swanson, CapFlex, and symptomatic OA. The FSMD passively moves the tested finger and registers the exerted torque during a preset angle sequence (safety threshold of ±0.2Nm). The slopes of the recorded torque-angle curves represent joint stiffness. Results Among a total number of 56 PIP joints, 12 were healthy, 3 replaced with a Swanson prosthesis, 19 CapFlex prosthesis and 8 symptomatic OA. Over all measured joints, PIP joint stiffness was lower in intermediate flexion positions and increased towards end positions of the joint (figure 1); e.g. median stiffness was 1.5Nmm/° [range 0.6-5.6], 1.7Nmm/° [0.5-18.9] and 3.3Nmm/° [1.0-15.7] at 50°, 30° and 90° PIP flexion, respectively. Within the set torque threshold, two fingers with a CapFlex prosthesis were not able to reach flexion angles ≤30°, while all three Swanson PIP did not reach flexion angles ≥90°. Discussion and Conclusion Measurement with the FSMD provides torque-angle data, which enables calculation of joint stiffness throughout the ROM of a finger`s PIP joint. We present the results in a small number of patients, offering preliminary data for the chosen, specific subgroup after PIP joint replacement surgery. PIP joints with a Swanson prosthesis tend to be less stiff in more extended positions and become considerably stiffer at finger flexion angles >60°. PIP joints with a CapFlex prosthesis tend to be particularly stiffer in more extended positions. Furthermore, this group showed a large variance for stiffness in the extended positions, i.e. while some could not even reach flexion angles of <30°, others delivered values equal to healthy joints. In a future perspective, measurement and a systematic analysis in a larger number of patients is required for the introduction of this novel method to assess and quantify finger joint stiffness. |
|
|
|
FM44
Can we correct hyperextension of the MCP joint with thumb CMC implant arthroplasty?
Vanessa Reischenböck, Zürich; Daniel Herren, Zürich; Jenny Imhof, Zürich; Miriam Marks, Zürich; Stephan Schindele, Zürich
DetailsAims: The primary objective was to examine whether thumb carpometacarpal (CMC) implant arthroplasty can correct hyperextension in the thumb metacarpophalangeal (MCP) joint. As a secondary outcome, clinical outcomes one-year post-surgery were compared between patients with and without MCP hyperextension. Methods: Patients treated with a thumb CMC implant arthroplasty (Touch®, KeriMedical, Switzerland) who were prospectively documented in a registry and had complete baseline and 1-year follow-up data were included. Hand function was assessed with the brief Michigan Hand Outcomes Questionnaire (brief MHQ, score 0-100). Key pinch strength was assessed with a pinch gauge and range of motion of the MCP joint with a goniometer. Differences between baseline and follow-up were analysed with the Wilcoxon signed-rank test. The outcomes of patients with a preoperative MCP extension of > 20° (hyperextension group) were compared to the outcomes of patients with ≤ 20° using the Wilcoxon rank-sum test. Results: We included 172 patients of whom 41 had a preoperative MCP hyperextension of > 20° and 131 patients had no hyperextension. In the hyperextension group, MCP extension was corrected from preoperative mean 33° (95% confidence interval CI: 31-35) to 10° (CI: 6-13) at 1 year (p≤ 0.001). Patients in the control group had a preoperative MCP extension of 10° (CI: 9-12) which was reduced to 5° (CI: 4-7) at 1 year (p≤ 0.001). Patients with preoperative MCP hyperextension had lower key pinch strength at 1 year compared to the control group (5.9 kg (CI: 5.3-6.6) vs. 7.0 kg (CI: 6.7-7.5), p≤ 0.01). The brief MHQ did not differ between the groups (85 (CI: 82-88) vs. 87 (CI: 82-92), p=0.7). Complications appeared in 29 patients of whom 7 had preoperative MCP hyperextension. No significant association between hyperextension and complications was observed (p=1.0). Conclusion: Thumb CMC implant arthroplasty can correct preoperative MCP hyperextension, and preoperative MCP hyperextension does not appear to increase complications. Therefore, we recommend using implant arthroplasty also in patients with hyperextension of the MCP joint, provided the joint is stably otherwise. |
|
|
|
FM45
2D/3D Analysis of the axis & angle for closing wedge-OT of the MC I for early-stage OA of the CMC I
Philipp Honigmann, Bruderholz; Marco Keller, Zürich; Mathias Häfeli, Chur; Jasmine Rüegg, Nethergate (GB)
DetailsPurpose The aim of this project is to define the necessary axes (anatomical, mechanical and adjacent joint axis) of the first metacarpal bone in order to calculate a first metacarpal tilt angle and to determine a correction angle to be used in a Wilson osteotomy. Material and Methods CT-scans of twenty healthy and six symptomatic patients were used to find a method to define the required axes. Once the axes were defined, the first metacarpal tilt angle could be determined. This value was compared between healthy and symptomatic data. The angle of the closing wedge in a Wilson osteotomy was the calculated and explained with the defined axes and the determined angles. The effect of a Wilson osteotomy was described based on these data. Results We defined and reproduced the anatomical, mechanical and a proximal joint axis. The angle between the anatomical and mechanical axis showed an average of 6.1° (SD 1.2°). An angle of 85.4 ° (SD 2.8°) between the proximal joint axis and the mechanical axis (metacarpal tilt angle mechanically) and 79.4° (SD 3.1°) for the anatomical axis (metacarpal tilt angle anatomically) was calculated. The proximal joint axis is angulated 9.6° (SD 4.6°) to the middle plane of the metacarpal one. There was no statistically difference between healthy and symptomatic preoperative MC I angles and axes. A mean angle of 28.7° (SD 5.2°) of correction was found in 6 symptomatic patients. Based on these data an angle of 22.6° (SD 2.5°) 1 cm and 26.7° (SD 2.5°) 1.5 cm above the proximal joint axis has been identified as optimal average correction angle for a Wilsons-osteotomy. A comparison between the mean values calculated based on 2D and 3D data showed no significant differences.
Conclusion The correction angle of 20°-30° determined by Wilson could be reproduced with the calculations and explained with the axes of the bone. However, the angle of correction is variable depending on the osteotomy height, bone thickness and angle between the axes. This newly developed method for calculating the angle of correction when performing a Wilson osteotomy can be used to improve the surgical technique and outcome. If the axes are defined with small adjustments on a lateral 2D X-ray, similar values can be calculated and a 3D data set is not necessarily required, which is more suitable for a daily clinical routine. |
|
|
|
FM46
3D analysis of the thumb after trapeziometacarpal joint surgery
Sophie Charlotte Brackertz, Zürich; Gabriella Fischer, Zürich; Maurizio Calcagni, Zürich; Lisa Reissner, Zürich
DetailsOsteoarthritis of the trapeziometacarpal joint (TMC) can effectively be treated surgically with Wilson osteotomy (WO), trapeziectomy with ligament reconstruction/tendon interposition (LRTI) and implant arthroplasty (TP). The aim of the study was to record the thumb motion during basic motion and 3 activities of daily living (ADL) in patients following WO, LRTI or TP using infrared cameras. Twenty-nine patients (max. 60 y/o) who had been treated with WO(n=10), TP(n=10) and LRTI(n=9) were recorded with a motion capture system during isolated abduction-adduction, flexion-extension (F/E), opposition and circumduction and three ADLs: opening a jar, bottle and key. Mean follow-up was 23 months (12-66). The patients subjective hand function was assessed with the MHQ. TMC range of motion (ROM) was calculated for each movement trial. Forces during each ADL were measured using a torque force device. Results are reported as median (range) and compared with a Kruskal-Wallis test (α=0.05). MHQ was similar in all groups with WO 78, TP 88, LRTI 84. During thumb opposition, TMC F/E ROM was significantly larger after WO (44°, 28-54°) compared to TP (28°,18-64°,p=0.038) and LRTI (30°,15-41°,p=0.026). During circumduction, TMC adduction-abduction ROM was significantly larger after TP (27°,13-46°) compared to LRTI (15°,12-28°;p=0.021), but not compared to WO (21°, 8-44°). In contrast, during isolated movements in the standard anatomical planes, no statistically significant difference was present. When opening a glass, patients after WO reached 125% of force compared to the contralateral side, after TP 100% and 85% after LRTI. For turning a key TP reached the highest forces.Total MHQ score was indicative of good to very good function, 3 patients indicated a fair function. Patients after LRTI had lower function in pinch force and ROM in basic movements compared with the other two groups. When comparing kinematics of patients after WO and TP during circumduction and opposition, WO allows more TMC movement in the F/E plane whereas motion in the radial-ulnar plane was larger after TP. These differences were not found during isolated movements in the anatomical planes. Force recordings during ADL compared to the contralateral side was highest in the WO group when opening/closing a jar,TP group reached highest forces in turning a key. For the kinetic parameters, patients after LRTI had the poorest outcome, while WO and TP showed advantages depending on the considered outcome. |
|
|
|
FM47
Health-Related Quality-of-Life in Symbrachydactyly: Balancing Function and Appearance.
Andreas Weber, Zürich; Patrizia Sulser, Zürich; Christopher Gaffney, Zürich; Marco Kaenzig, Zürich; Daniel Weber, Zürich
DetailsHYPOTHESIS In children with symbrachydactyly, we hypothesized that the highest Pediatric Quality-of-Life Inventory (PedsQL) scores would be found in patients with the most severe forms. Further, we posited that non-significant differences would be observed in assessments of patients' Health-Related Quality-of-Life (HRQoL), appearance, and perceived function compared to their parents.
METHODS In this single-center, observational study, all symbrachydactyly patients treated from 2000 to 2018 were invited to participate. Patients (≥3y) and their parents were asked to complete questionnaires on HRQoL (PedsQL), appearance (ZASH, Zurich Appearance Score for Hands), and function (CHEQ, Children's Hand-use Experience Questionnaire). Patients were assigned to groups based on their ability to grasp. Group A: good grip (unrestricted/slightly impaired grip), Group B: pinch only, Group C: no grip/pinch capability.
RESULTS We included 58 patients/parents (male 60%; median age 8.5 years [range 3-26]). All symbrachydactyly types were represented and categorized (Group A [n=18; 31%], Group B [n=15; 26%], Group C [n=25; 43%]). Overall PedsQL scores were high (median 89.1) and similar between genders (M 90.2; F 89.1). Compared to the reference sample, no significant difference between overall scores was detected (95% CI, -0.9 to 4.4; p=.23). For the PedsQL sub-scales, patients consistently rated their perceived function as highest (median 93.8) and emotional sub-scale as lowest (median 87.5). When grouped by hand function, PedsQL scores were lower in Group B (median 85.2) compared to Group A (median 91.3) and Group C (median 92.4). When comparing patient/parent assessments, parents assessed the emotional sub-scale significantly lower (95% CI, -10 to -2.5; p=0.01). ZASH scores were higher in patients (median 59.5) compared to parents (median 54.0), whereas CHEQ scores were concordant. ZASH scores did not correlate with either the CHEQ or PedsQL, while the CHEQ moderately correlated with PedsQL scores (r=0.53-0.68), but only in the parent sample.
CONCLUSIONS Overall, patients with symbrachydactyly and their parents reported consistently high HRQoL scores. Patients without grip capability had the highest PedsQL scores. The differences in PedsQL scores between parents and patients were similar to those in the reference group. ZASH and CHEQ scores were similar between patients and parents. Neither hand function nor appearance were found to have appreciable correlations with the PedsQL. |
|
|
|
FM48
Management of trapezium’s palmar osteophyte in trapeziometacarpal joint osteoarthritis
Julie Mercier, Lausanne; Lucille Auberson, Sierre; Romain Baillot, Lausanne; Anton Raemy, Lausanne; Swenn Maxence Krähenbühl, Siders; Nicolas Balagué, Sierre
DetailsBackground: Trapeziometacarpal (TMC) joint osteoarthritis is a frequent degenerative pathology encountered in hand surgery. Arthroplasty through a dorsal approach is a routine surgical procedure with satisfactory results, including significant pain reduction and improvement of functional thumb range of motion. However, some patients report persisting post-operative pain on the thenar eminence over the trapezium. It can be explained by an overseen palmar osteophyte of the trapezium, which could not be identified on preoperative plain radiographs nor during the surgical procedure but can only be assessed on a CT scan. To the best of the authors’ knowledge, limited studies have evaluated the degenerative aspect of trapezium, and particularly the osteophytic development on the palmar side. Overlapping of carpal bones on plain radiographs does not allow a proper analysis of trapezium osteophytes on its palmar side, resulting sometimes in incomplete surgical treatment. Indeed, this osteophyte can be responsible for persisting pain despite the adequate management of TMC osteoarthritis. Methods: Starting from 2021, we systematically looked for palmar tenderness over the trapezium during our routine clinical examination of patients suffering from TMC osteoarthritis. If the clinical exam was positive, a complimentary CT was realized to assess the aforementioned osteophyte. When present, we added to our usual surgical procedure for arthroplasty a palmar approach to excise the osteophyte, sometimes using 3D printing of the trapezium for preoperative planning. Results: Our study involves 12 patients suffering from TMC osteoarthritis with an additional symptomatic palmar osteophyte, clinically suspected and detected on CT scan. The excision of this osteophyte through a palmar approach led to a resolution of the specific palmar pain. Conclusion: The knowledge of this possible symptomatic palmar osteophyte changed our therapeutic procedure. The standard surgical dorsal approach of the TMC does not allow visualization of the palmar side of the trapezium and consequently the presence of a palmar osteophyte, whose persistence precludes satisfactory postoperative pain evolution. This allowed us to develop a new algorithm for the treatment of TMC joint osteoarthritis. We now systematically include a CT-scan when palmar tenderness is present over the trapezium of a patient suffering from TMC osteoarthritis, allowing the proper treatment to a poorly known source of persisting pain. |
|
|
|
FM49
Collagenase versus limited fasciectomy for Dupuytren’s disease – early postoperative implications
Julia Bernhard, Bern; Rémy Liechti, Bern; Dominique Merky, Bern; Ramin Ipaktchi, Bern; Esther Vögelin, Bern
DetailsIntroduction Since the withdrawal of the market authorisation of Collagenase clostridium histolyticum (CCH) in Europe in March 2020, the value of this treatment option in Dupuytren’s disease became more evident. The aim of this study was to compare outcomes of patients receiving CCH injection with patients undergoing limited fasciectomy (LF) with focus on the early postoperative soft tissue conditions and individual burden measured by the frequency of surgeon and hand therapy visits. Materials and methods All consecutive patients undergoing either CCH injection or LF as a first line treatment in a 15 year period (2006-2021) at the University Hospital of Bern, Switzerland were assessed for eligibility. Propensity score matching involving confounding factors (age, gender, diabetes, family history, disease severity and number of rays involved) was performed to minimize selection bias. Primary outcome analysis was focused on the early postoperative soft tissue condition of the hand using a local wound score with points given for hyperaemia, tenderness and scar mobility. Secondary outcomes included the number of medical and hand therapy visits. Results In the mentioned timeframe, 195 patients were treated for Dupuytren’s disease at the University hospital of Bern. After exclusion and propensity score matching, two treatment groups of 32 patients each were formed. Mean age was 69.7 years (range 42-85 years) in the CCH group and 70.4 years (range 40-91 years) in the LF group. There were no significant differences in baseline characteristics between treatment groups. Correction of extension deficit was comparable in both treatment groups. Local wound score was significantly worse in the LF group than in the CCH group (mean 0.47 vs. 0.09 points, MD 0.38, 95% CI [0.15, 0.60], p = 0.002). The number of surgeon and hand therapy visits was significantly higher in the LF group (mean 4.7 vs. 1.9 visits, MD 2.8, 95% CI [1.8, 3.8], p < 0.001 and mean 14.6 vs. 4.4 visits, MD 10.2, 95% CI [4.2, 16.1], p = 0.004, respectively). Conclusion Evidence of the present study suggests that patients undergoing CCH injection have a significantly less complicated wound healing with softer scar conditions requiring less intensive surgical and hand therapy aftercare. In our opinion, CCH treatment is an important tool in the armamentarium for the treatment of Dupuytren's disease and the reintroduction or approval of a generic drug worthy of being supported. |
|
|
|
10:00 – 11:30
|
Hauptsession IVRéduction sous scopie des fractures digitales: apport des attelles thermo-formées |
|
|
Theatersaal
HS4
|
Swenn Maxence Krähenbühl, Siders; Myriam de Ieso, Siders
|
|
Revue de la littérature sur la prise en charge chirurgicale des fractures de phalanges
Marie-Aimée Päivi Soro, Lausanne
|
|
|
Revue de la littérature sur les attelles faites en post réduction de fractures digitales
Magaly Favre, Siders
|
|
|
Présentation de la procédure de réalisation d’attelle post réduction sous scopie à l’hôpital de Sierre + cas cliniques
Magaly Favre, Siders; Myriam de Ieso, Siders
|
|
|
La prise en charge des fractures de phalanges en Afrique
|
|
|
|
10:00 – 11:30
|
Workshop B |
|
|
Club Casino
WSB
|
Tamara Hauri, Bern
|
|
Medical Flossing in der Handtherapie
Nicole Plüss, St. Gallen; Susanne Habelt, St. Gallen
|
|
|
|
11:30 – 13:00
|
Stehlunch – Begegnung in der Ausstellung |
|
|
11:45 – 12:30
|
Mittags-Symposium |
|
|
Theatersaal
|
||
MARIS B|flow – so dokumentieren Sie morgen!
Urs Niklaus Genewein, Rheinfelden; Dirk Hüske-Kraus, Illingen (DE)
Sponsoren
|
|
|
|
11:45 – 12:30
|
Praxisinhaber:innen-meeting |
|
|
Ballsaal
PIM
|
Julie Dziwornu, Aarberg; Patricia Kammermann, Bern; Stéphanie Rosca-Furrer, La Chaux-de-Fonds; Ursula Osterwalder, Baden; Barbara Roland, Miège; Pauline Chèvre, Fribourg; Lea Feller, Winterthur; Barbara Aegler, Zürich
|
|
Inputreferat
Barbara Aegler, Zürich
|
||
|
13:00 – 14:30
|
Freie Mitteilungen IV |
|
|
Ballsaal
SGHR-FM4
|
Sabrina Koch-Borner, Nottwil; Jürgen Busskamp Waldvogel, Pratteln
|
|
|
FM75
Relative Motion for Limited Finger Joint Mobility: Understanding Applications and Decision-Making
Sarah Ewald, Zürich
DetailsRelative motion (RM), initially introduced by Merritt et al. (2000) for the treatment of surgically repaired extensor tendons, has since been utilized in the management of various finger joint conditions such as flexion or extension limitations, trigger fingers, boutonniere deformities, and post-operative rehabilitation of flexor tendon repairs. One big advantage of relative motion orthoses (RMO) versus tradtional splinting is that it allows the finger to move while influencing motion, this in turn means that the hand remains functional while wearing the RMO and thus can be worn for longer periods of time during hand activity. This paper explores the versatility of relative motion flexion and extension and addresses the critical question of when and how therapists should employ these techniques for finger joints with limited motion and when other techniques should be utilized. A comprehensive algorithm has been developed to aid in this decision-making process, which guides therapists in evaluating and selecting appropriate treatment options. In addition to thermoplastic splints, alternative relative motion placement methods and splint options will be presented, with case examples from clinical practice. Furthermore, this presentation will delve into other pertinent considerations for therapists, including determining the number of fingers to include in the relative motion orthosis, the differential of relative motion, and the duration of splint usage. Merritt, WH, Howell JW, Tune R, et al. Achieving immediate active motion by using relative motion splinting after long extensor repair and sagittal band rupture with tendon subluxation. Oper Tech Plast Reconstr Surg 2000;7: 31–37 https://doi.org/1053/oa.2000.5972 |
|
|
|
FM76
Massgefertigte Lederschienen für manuell tätige Patient:innen bei Handgelenkschmerzen
Ramona Ziörjen, Burgdorf; Karin Lüthi, Zollbrück
DetailsHintergrund: Arthrose ist die häufigste Gelenkserkrankung (Rheumaliga Schweiz, 2023) und schränkt insbesondere manuell tätige Menschen ein. Für diese kann eine Handgelenksschiene entlastend wirken. Es gibt nur wenig Literatur über massgefertigte Handgelenksschienen aus Leder (Haskett et al., 2004; Thiele et al., 2009). Im Vergleich zu vorgefertigten Schienen, zeigen die massgefertigten Lederschienen jedoch gute Resultate bezüglich Schmerzreduktion und Betätigungsperformanz. Ziel: Ziel war es, Lederschienen für manuell tätige Personen mit Handgelenksbeschwerden in unserer Praxis herzustellen. Dazu gehörte eine Anleitung, Schulung einiger Mitarbeitenden und Herstellung der Schienen für individuelle Patient:innenbedürfnisse und deren betätigungsorientierten Ziele. Methodik: Eine systematische Literaturrecherche in verschiedenen Datenbanken wurde durchgeführt, um die Evidenz von massgefertigten Lederschienen bei Arthrose zu ermitteln. Zusätzlich wurde durch Austausch mit vier Ergotherapeutinnen Erfahrungswissen über die Herstellung von Lederschienen gesammelt, zusammengetragen und weiterentwickelt. Resultat: Eine massgefertigte Lederschiene hat sich für manuell tätige Patient:innen mit anhaltenden Handgelenksschmerzen als vorteilhaft erwiesen, denn sie ist schmerzlindernd, bequem, belastbar, praktisch und ermöglicht Aktivität. Implikation für die Praxis: Lederschienen sind für manuell tätige Patient:innen mit Handgelenksschmerzen eine gute Alternative zu vorgefertigten Schienen und können in einer handtherapeutischen Praxis mit entsprechender Anleitung preiswert hergestellt werden. Haskett, S., Backman, C., Porter, B., Goyert, J. & Palejko, G. (2004). A crossover trial of custom-made and commercially available wrist splints in adults with inflammatory arthritis. Arthritis and rheumatism, 51(5), 792–799. https://doi.org/10.1002/art.20699 Rheumaliga Schweiz. (2023, 14. März). Arthrose - Rheumaliga Schweiz. https://www.rheumaliga.ch/rheuma-von-a-z/arthrose Thiele, J., Nimmo, R., Rowell, W., Quinn, S. & Jones, G. (2009). A randomized single blind crossover trial comparing leather and commercial wrist splints for treating chronic wrist pain in adults. BMC musculoskeletal disorders, 10, 129. https://doi.org/10.1186/1471-2474-10-129 |
|
|
|
FM77
3D printing and hand rehabilitation : our experience
Francesca Ferrario, Lugano; Susanna Pagella, Lugano; Mario Gaetano Fioretti, Lugano; Marco Guidi, Gravesano
DetailsIntroduction: Three-dimensional (3D) printing is a relatively new and quickly growing method of manufacturing in healthcare (1). This technology gives hand therapists a remarkable tool to make “in-house” assistive devices, hand exercise equipment, therapy tools, orthotic components, medical tools and more. Considering the described advantages of this technology we decided to use it in our practice. 3D printing involves acquisition, preparation and printing, whereby materials are joined, layer by layer to manufacture 3D-printed model. Objective: 3D printing is a cost-effective technology that can replicate commercially available items or customize new ones. The increasingly lower cost of 3D printing materials and the absence of the need to monitor the 3D printer during printing means that this technology can be successfully integrated into clinical practice(2). The ease customization and ability to locate various online design options further enables client- centered practice. Method: We design and print ten therapeutic aids, such as instruments for proprioception , hand strengthening and dexterity. For patient education, we print 3D printable upper limb bones. Once printed, the bones can be articulated to simulate joint motion. For further patient education, other materials can be added to the bone anatomy model to show the anatomy and kinesiology of muscles, tendons, and nerves. The material that we use is Polylacticacid (PLA) which is the most popular material in the 3D printing due to its biodegradability and low-toxicity, with fused deposition modeling (FDM). Discussion: In our opinion, the benefits of 3D printing are the replicability of 3D printed devices that provides quick and easy access for therapists and patients. In particular 3D printed devices can be custom made for a patient based on their individual need and it is feasible for a therapist to learn how to use a 3D printer with minimal training and instructions. There are also limitations in using 3d printing such as the need for a dedicated print area because some materials creates mild toxic fumes while printing as ABS. In addition some materials are non-biodegradable and some technologies and materials still requires very expensive printers. Dodziuk, 2016. Hunzeker&Ozelie, 2021. |
|
|
|
FM78
Die Rolle der Handtherapie beim 3D-Druck von Schienen im Akutspital
Christa Wyss, Basel; Christina Furthmüller, Basel; Lorena Schrepfer, Basel
DetailsThema:Schienen gehören seit jeher zum Fachgebiet der Ergo- und Handtherapie und werden individuell an den Patienten angepasst. In den letzten Jahren hat sich die Technologie des 3D-Drucks stetig weiterentwickelt und ermöglicht auch die Herstellung von Handorthesen. In diesem Vortrag soll es um die Frage gehen, ob diese Möglichkeit auch im Akutspital eingesetzt werden kann und welche Rolle die Handtherapie dabei spielt. Dafür werden die Erkenntnisse einer bereits publizierten Studie herangezogen. Eine perfekt angepasste Schiene kann zu einem höheren Tragekomfort und einer besseren Compliance führen. In einer randomisierten Studie wurden 3D-gedruckte Schienen mit konventionell angepassten thermoplastischen Schienen verglichen. Ziel dieser Pilotstudie war es, zu untersuchen, ob die Herstellung von Schienen mittels 3D-Druck auch im klinischen Umfeld erfolgreich durchgeführt werden kann. Durchführung: Die Handtherapeut*innen hatten die Aufgabe, ihr fundiertes Wissen zum Schienenbau an die Studienärztin weiterzugegeben. Sie hatten eine verantwortliche Rolle bei der Erstellung eines neuen Prozesses zum 3D-Druck; sie waren involviert in die interdisziplinäre Aufbietung der Patient*innen, den 3D-Scan der Hand, das Anpassen der vorbereiteten Schienen und die Erhebung von Daten. Die Studie umfasste 20 Patient*innen (10 Kontrollgruppe/10 Interventionsgruppe), die eine Schiene für mindestens 4 Wochen tragen mussten, wobei das Schienenformat nicht relevant war. Der Komfort und die Zufriedenheit der Patient*innen wurden mit Hilfe eines Fragebogens bewertet, der während der Anpassung der Schiene sowie zwei Wochen und vier bis sechs Wochen später von der Handtherapie durchgeführt wurde. Schliesslich wurde die Anwendung im klinischen Umfeld und die möglichen Vorteile des 3D-Druckverfahrens evaluiert. Ergebnis: Schienenherstellung mittels 3D-Druck ist im Akutspital möglich. Das spitalinterne Vorgehen kann noch verbessert werden. Die Handtherapeut*innen hat im Prozess des 3D-Schienendrucks eine zentrale Aufgabe. Sie könnte jedoch in einem zukünftig implementierten Prozess noch mehr Verantwortung übernehmen. Die Patientenzufriedenheit war in beiden Gruppen auf einem hohen Niveau. Weitere Themen, die in aufbauender Forschung beleuchtet werden sollten, sind PROMs (Patient-related Outcome Measures), funktionelle Outcomes und eine Kosten-Nutzen-Analyse. |
|
|
|
FM79
Athletes-Centered: splint creativity in sports hand rehabilitation.
Mario Gaetano Fioretti, Lugano; Francesca Ferrario, Lugano; Susanna Pagella, Lugano; Marco Marano, Manno
DetailsBackground: Approximately 25 % of all sports-related injuries involve the hand or wrist. Due to the high level of physical demand for function, athletes represent a unique subset of the population.1 Rehabilitation of athletes is particular because the type of injury has both physical and psychological aspects.2 For Europe, according to a study3 based on the year 2018 in Germany (EU Injury Database) at the epidemiological level, hand and wrist injuries are more frequent for: sports without a bat (31%), cycling (28%), equestrian sports (13%), winter sports (7%) and martial arts (6%). In most cases athletes need standard splints for the period of immobilization or protection. There are exceptions where the splint is not standardly available on the market or the hand therapist is required to invent splints adapted to the individual and functional needs of the athlete while having to maintain the same safety standards. Method: The new paradigm of evidence-based practice (EBP)4 puts the patient at the center of the discussion along with the practitioner's experience and skill and the integration of the best clinical evidence. Therapist creativity, scientific evidence, sports physician experience and athlete-centered approach become the key to success. We provide 5 case reports with 4 innovative patient-centered splints design. We assess the VAS score before and after the wearing of the splint in a training setting and the PSQ-18 score to assess their satisfaction of the splint and the taking care part. Results: The active protective splints proposed were a compensatory tool to achieve an early return working both to functional and psychological aspects. The proposed splints resulted in athletes returning to sport as early as hoped. The functional results shows a decrease in pain about 70% in VAS score and an the highest level of patient satisfaction assessed with the PSQ-18 score. Consequently with the splints the athletes received custom rehabilitation programs. Discussion: Careful multidisciplinary assessment, transparent exchange of information, and active listening to the athlete makes it possible to identify the best effective and safe solution. This presentation is a personal experience opinion aimed at suggesting new splint’s options and designs and stimulating constructive discussions. Avery III et al, 2016 Lucchetti R., Pegoli L., Bain G.I., 2018 Stogner et al., 2020 Guyatt G.H., Rennie D., 2002 |
|
|
|
13:00 – 14:15
|
Special SessionHong Kong Society for Surgery of the Hand and Hong Kong Society for Hand Therapy |
|
|
Theatersaal
SS
|
Mavis Man Hei Lee, Hong Kong (HK); Siu Cheong Jeffrey Justin Koo, Hong Kong (HK); Stephan Schindele, Zürich; Ursula Osterwalder, Baden
|
|
PIPJ Replacement - Asian Perspective
Ping Tak Chan, Hong Kong (HK)
|
|
|
Arthroscopic 1st CMCJ Fusion: The Hong Kong Experience
Esther Ching San Chow, Hong Kong (HK)
|
|
|
CIND in Distal Radius Fracture
Margaret Woon Man Fok, Hong Kong (HK)
|
|
|
Historical and Cultural Perspective of Hand Surgery Development in Hong Kong
Siu Cheong Jeffrey Justin Koo, Hong Kong (HK)
|
|
|
Comparison of Mini-open Anterior Transposition and Medial Epicondylectomy in Cubital Tunnel Syndrome
Michelle Syn Yuk Lee, Hong Kong (HK)
|
|
|
Clinical Outcome of Failed 1st CMCJ Fusion
Edmund Leung Kai Yau, Hong Kong (HK)
|
|
|
Introduction of the Hong Kong Society for Hand Therapy
Mavis Man Hei Lee, Hong Kong (HK)
|
|
|
Education on Occupational Therapy in Hand Rehabilitation
Josephine Wong, Hong Kong (HK)
|
|
|
|
13:00 – 14:00
|
Workshop C |
|
|
Club Casino
WSC
|
Ingrid Cianci, Affoltern am Albis
|
|
Die Relative Motion Schiene: klein, fein und effizient!
Anita Gisi, Zürich; Isabelle Frank-Ziem, Zürich
|
|
|
|
14:15 – 14:30
|
Report Fonds Verdan |
|
|
Theatersaal
RFV
|
Ivan Tami, Lugano
|
|
Fellowships in Melbourne und Sydney
Lea Estermann, Zürich
|
||
Fellowship periphere Nervenchirurgie: St. Louis/USA
Stefanie Hirsiger, Bern
|
||
|
14:30 – 15:00
|
Kaffeepause |
|
|
15:00 – 16:30
|
Hauptsession VBattle of the Masters |
|
|
Theatersaal
HS5
|
David Jann, Thun; Florian Früh, Aarau; Esther Bohli, Biel/Bienne
|
|
Fuse or replace - what’s right for osteoarthritis of the wrist?
Philipp Honigmann, Bruderholz; Mathias Häfeli, Chur
|
||
Tendon transfer vs nerve transfer for PROXIMAL radial nerve palsy
Pascal Ducommun, Zürich; Olga Politikou, Zürich
|
||
Therapiehäufigkeit, Abschluss Behandlung - welche Kriterien und Bedürfnisse von Patient*innen, Ärzt*innen und Therapeut*innen leiten uns?
Christa Greminger, Zug; Bettina Juon, Bern; Reto Fuhrer, Biel; Marisa Zumbrunn, Basel
|
||
|
16:30 – 17:00
|
Awards ceremony & Schlusspunkt |
|
|
Theatersaal
AWC
|
||
SGHR-Award
Atena Bosi, Payerne; Christa Greminger, Zug; Michael Haller, Solothurn
|
||
Gong Show Award
Thomas Mészáros, Fribourg
|
||
GFCA Award
Thomas Mészáros, Fribourg
|
||
Poster Award
Thomas Mészáros, Fribourg
|
||
Schlusspunkt
Ivan Tami, Lugano; Maurizio Calcagni, Zürich; Patricia Kammermann, Bern; Stéphanie Rosca-Furrer, La Chaux-de-Fonds
|